The incidence of Anterior Cruciate Ligament (ACL) reconstruction amongst pediatric patients has risen over the last decade [1]. Injuries to the ACL can result in ligament rupture or, less commonly, traumatic avulsion fracture at the ACL insertion site on the proximal tibia. Postoperative pain control after ACL reconstruction or repair usually involves opioids. Adult literature demonstrated daily opioid consumption of 35-45 mg morphine equivalents in the first 2 weeks after ACL reconstruction [2]. Regional anesthesia has proven to reduce nociceptive pain and opioid requirements following ACL surgery, thereby facilitating earlier hospital discharge and improved patient satisfaction [3-5].
Widely used for knee surgery, the Adductor Canal Block (ACB) provides motor-sparing analgesia to the anteromedial knee and distal medial leg [2,4,6]. However, its lack of posterior knee and anterolateral coverage makes it non-ideal as a sole agent. The ultrasound-guided deposition of local anesthetic to the Interspace between the Popliteal Artery and The Posterior Knee Capsule (IPACK) in combination with blockade of the anterior knee with an ACB has gained significant interest for such surgery [7,8]. Herein we describe the utilization of the IPACK combined with an ACB for arthroscopic ACL repair in a pediatric patient.
A 10-year old, 41kg, healthy male presented following a motor vehicle injury. Imaging revealed left ACL avulsion from its tibial attachment, anterior-lateral meniscus tear and avulsion of the popliteofibular ligament. He underwent arthroscopic assisted repair of the proximal tibial avulsion fracture. Proceeding general anesthesia, the patient was positioned supine with the left lower extremity externally rotated and flexed 40 at the knee. A high-frequency linear ultrasound probe (15MHz) was placed transverse to the medial thigh, and rotated medially to visualize the adductor canal for ACB. A 22-gauge 50 mm echogenic needle was advanced in-plane from the lateral to medial direction, deep to the sartorius and juxtaposed to the vastus medialis. Following negative aspiration, 6ml of bupivacaine 0.25% with preservative-free clonidine 20mcg was deposited in the adductor canal. A curvilinear, low-frequency transducer (2-5MHz) was used for the IPACK to maximize visualization. With the patient in the same position, the probe was placed in the popliteal fossa identifying the popliteal artery and femoral condyles. The probe was then advanced cephalad until the shaft of the femur was visualized. A 22-gauge 80 mm echogenic needle was advanced in-plane, deep to the popliteal artery and above the joint capsule. Following negative aspiration, 10 ml of bupivacaine 0.25% with preservative-free clonidine 20mcg was deposited (Figure 1). Both ACB and IPACK single shot nerve blocks were performed in 6 minutes.
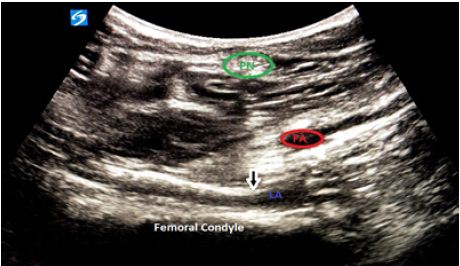
Figure 1: IPACK blockade with arrow highlighting needle in-situ. Femoral Artery (FA), Popliteal Nerve (PN), Local Anesthetic (LA).
After the patient was prepped and draped, the anatomic landmarks of the anteromedial and anterolateral portals were identified. Additional short-acting local anesthetic (lidocaine 1% with epinephrine 1:200k) was administered by the surgeon at the anterolateral and anteromedial port sites. The arthroscope was introduced through the anterolateral portal. Systematic arthroscopic evaluation revealed a displaced tibial spine fracture with the ACL attached to a fragment and hinging of the anterior aspect of the fracture with intermeniscal ligament interposition. The intermeniscal ligament was extracted and the fracture bed was debrided. The sutures were secured to the ACL base and then secured to the donor site of the fracture with push lock anchors. There was successful fixation after anchor placement. The patient was maintained on 1 MAC of sevoflurane and received a total of 1.5 mg/kg of ketamine given in divided doses; no intraoperative opioids were required. The total operative time was 89 minutes. The procedure was uneventful and there were no apparent complications. The estimated blood loss was minimal.
In the immediate post-operative period the child’s numeric pain score was 4/10. Pain was isolated to the anterior lateral port site, for which 0.02 mg/kg (1mg) of morphine was administered. Physical exam revealed no sensation to light touch on the anteromedial or posterior knee with preserved plantar-dorsiflexion at the ankle. On 24-hour outpatient follow-up, parents reported good pain control without motor weakness. He received one dose of an oral acetaminophen-opioid preparation approximately16 hours from discharge. There was no evidence of block complication.
Arthroscopic tibial spine fracture repair usually involves medial and lateral parapatellar portals. The tibial spine is fixed via sutures or screws. The ACL emerges from the medial and anterior tibial plateau coursing superiorly to its posterior insertion site along the posterior lateral femoral condyle. As such, surgical manipulation can impose both anterior and posterior capsule knee pain. The ACB reproducibly offers similar anterior knee analgesia when compared to a femoral nerve block while avoiding quadriceps weakness, which allows faster ambulatory recovery and discharge [6,7]. IPACK targets the articular branches originating from the tibial and obturator nerves that travel through a tissue space between the popliteal artery and the femur. It provides posterior knee capsule analgesia by blockade of the obturator, tibial and common peroneal sensory innervation while sparing the motor effect observed with a sciatic nerve block, thereby maintaining the sensorimotor function of the leg and foot.
As evident in a cadaveric study, local anesthetic delivered via IPACK spreads throughout the popliteal fossa without proximal sciatic involvement [8], albeit extension to the common peroneal and tibial nerves was plausible. Combining the ACB and IPACK, opioid-sparing effect can be achieved for ACL repair or reconstruction while preserving motor function. This concept harmonized with the adult literature where reduction of morphine equivalent consumption and faster ambulatory discharge were noted with the addition of an IPACK block for ACL repair [9]. Our experience demonstrated motor-sparing effect and adequate analgesia with the IPACK and ACB combination for a pediatric patient undergoing ACL repair. While the adult literature and our observation suggests promising results, there are no studies that have investigated the safety and efficacy of IPACK block among pediatric patients undergoing knee surgery. Future investigation into the role of the IPACK block for ACL repair in pediatric patients is required.
References
- Ellis HB, VandenBerg C, Beck J, Pennock A, Pennock A, Cruz AI, et al. (2019) Trends in pediatric anterior cruciate ligament reconstruction: A review of surgeon fellowship, geography, and meniscus surgery in the ABOS part 2 database. Orthopc J Sports Med. [crossref]
- Barnett S, Murray MM, Liu S (2020) Resolution of pain and predictors of postoperative opioid use after bridge-enhanced anterior cruciate ligament repair and anterior crucial ligament reconstruction. Arthrosc Sports Med Rehabil 2: 219-228.
- Iskandar H, Benard A, Ruel-Raymond J, Cochard G, Manaud B, et al. (2003) Femoral block provides superior analgesia compared with intra-articular ropivacaine after anterior cruciate ligament reconstruction. Reg Anesth Pain Med 28: 29-32. [crossref]
- Abdallah FW, Whelan DB, Chan VW, Prasad GA, Endersby RV, et al. (2016) Adductor canal block provides noninferior analgesia and superior quadriceps strength compared with femoral nerve block in anterior cruciate ligament reconstruction. Anesthesiology 124: 1053-1064. [crossref]
- Koh IJ, Chang CB, Seo ES, Kim SJ, Seong SC, et al. (2012) Pain management by periarticular multimodal drug injection after anterior cruciate ligament reconstruction: A randomized, controlled study. Arthroscopy 28: 649-657. [crossref]
- Ludwigson JL, Tillmans SD, Galgon RE, Chambers TA, et al. (2015) A comparison of single shot adductor canal block versus femoral nerve catheter for total knee arthroplasty. J Arthroplasty 30: 68-71. [crossref]
- Kim D, Beathe J, Lin Y, Goytizolo E, Oxendine J, et al. (2019) The addition of ACB and IPACK to PAI enhances postoperative pain control in TKA: A randomized controlled trial. Anesth Analga 129: 526-535.
- Niesen AD, Harris DJ, Johnson CS, Stoike DE, et al. (2019) Interspace between Popliteal Artery and Posterior Capsule of the Knee (IPACK) injectate spread: A cadaver study. J Ultrasound Med 38: 741-745. [crossref]
- Huang A, Singh PA, Woon KL (2020) Interspace between the popliteal artery and the capsule of the knee (IPACK) block for anterior cruciate ligament reconstruction surgery: A two case series. Open Journal of Anesthesiology 10: 134-143.