Abstract
Mondor’s disease of the breast is a superficial thrombosis most often affecting the subcutaneous vessels of the anterior or lateral chest wall.
It is a rare pathology with less than 500 cases described in the literature.
The diagnosis is essentially based on physical examination. Ultrasound confirms diagnosis by visualizing the affected vein. Spontaneous evolution is always favorable.
Apart from the breast, other localizations are possible, particularly in the penis, abdomen and arm.
Through two cases supported in our structure, we present a review of the literature on clinical characteristics and on management.
Keywords
Mondor – Breast – Thrombosis
Introduction
Mondor’sDisease (MD) of the breast is characterized by superficial sclerosing thrombophlebitis of the subcutaneous veins of the anterior or lateral thoracic wall first described in 1939 by Henry Mondor. It generally involves one of this three veins: lateral thoracic, superior epigastric or thoracoepigastric (the most common) [1]. It has also been described in the arm, abdomen or penis [1, 2].
Its etiopathogenesis is not clearly defined. Referring to the few cases described in the literature, the development of this pathology would be reported after intense physical activity, pregnancy, trauma, surgical intervention (breast reconstruction, breast biopsy, oncological surgery, etc.) and various diseases (neoplasia , breast infection, inflammatory process) [1, 2, 3].
The diagnosis is essentially based on physical examination. We generally find a painful cord with the form of a groove, a straight gutter or, on the contrary, a linear relief. There is a particular “reticular” shape with the coexistence of two more or less parallel cords. The cord size is variable, from a few millimeters to several centimeters. It has a fibrous, indurated consistency and is located under the dermis [3, 4]. Breast ultrasound is the reference examination to confirm the diagnosis and finds the usual signs of venous thrombosis (non-compressibility of the vein under the probe and hypoechogenicendoluminal image) [4]. These symptoms persist for one to two weeks and disappear spontaneously or under symptomatic treatment.
Due to the rarity of this pathology in our countries, we report two cases collected from the Senology unit of the Gynecological and Obstetric Clinic of Aristide Le Dantec Hospital and a review of the literature to better understand this pathology.
Case report
Case 1: Mrs. S.B., 43 years old with no particular thrombotic history, had consulted for right mastodynia occurring intermittently following a fall from its height with reception on the right breast two years ago.
After her trauma, the patient would have noted recurrent pushes in the form of a very apparent and painful tubular formation in the breast which had motivated a consultation. The ultrasound found a superficial tubular formation with pseudo-cystic dilation above the nipple corresponding to a probable Mondor phlebitis. A breast MRI performed subsequently found a dilation of a supero-external superficial vein close to the nipple associated with a thickening of the skin suggesting Mondor’s disease. The spontaneous evolution was characterized by a progressive volume increase of the right breast passing from a cup B to a cup D.
The examination found a right breast increased in volume; the right supra-nipple superficial vein was very apparent, indurated and very sensitive. There was a sensitive homolateral axillary lymphadenopathy. Spontaneous evolution was favorable.
Case 2: Mrs. G.F., 34 years old has been followed in our service for 03 years for left breast cancer. The tumor was initially classified T2N1M1 (pulmonary).
Chemotherapy had been initiated with an anthracycline-based protocol and then she subsequently benefited from a conservative surgery such as tumorectomy with axillary dissection.Fifteen months after the intervention, there was a cancer progression which motivated the resumption of chemotherapy followed by a total mastectomy.
She presented, 15 days after the left mastectomy, a right mastodynia sitting at the external quadrant.
The physical examination found a painful cord measuring approximately 7 cm, located at the Supero-External Quadrant (SEQ) of the right breast (Figure 1) very suggestive of Mondor’s disease. Lymph nodes were free.
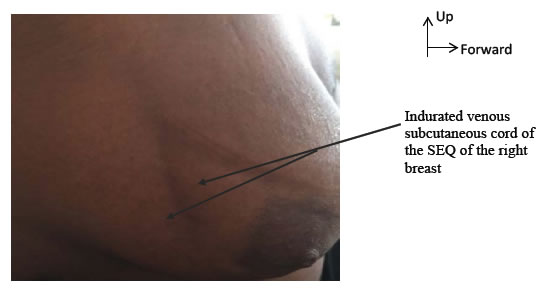
Figure 1. Painful indurated cord of the SEQ of the right breast in favor of Mondor’s disease
The ultrasound performed found a dilated incompressible superficial breast vein without any endoluminal image (Figure 2). There was no associated breast mass identified by mammography.
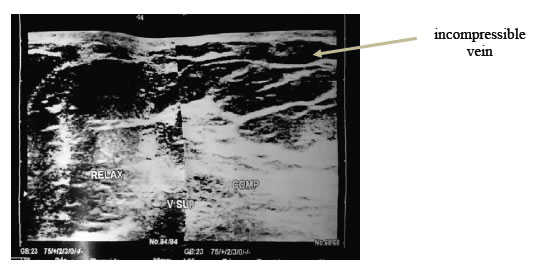
Figure 2. Ultrasound appearance in favor of a Mondor’s disease of the right breast with the presence of an incompressible superficial vein.
Treatment with non-steroidal anti-inflammatory (NSAIDs) drugs had been recommended with resolution of the pain and disappearance of the indurated cord after 10 days.
Discussion
Mondor’s disease, more commonly known as subacute subcutaneous trunculitis of the anterolateral chest wall, is a rare superficial thrombosis most often affecting the subcutaneous vessels of the anterior or lateral chest wall [1, 5].
The first reported case dates back to the end of the 19th century, but it was only in 1939 that Henry Mondor clearly reported a series of cases with a precise description of the physical symptomatology [6].
It is a rare affection with less than 500 cases described in the literature. The actual prevalence is unknown, only a few authors have reported an incidence of this affection which is between 0.5 and 0.8%. However, this affection is probably underestimated due to its mild nature with spontaneous resolution within a few days which means that patients do not always consult [6, 7].
The clinical form the most frequently found is chest wall and breast vessels damage as it was the case for our two patients.
Other localizations have been described like Mondor’s disease of the penis, the abdominal wall and the axillary space [1, 2, 8].
Despite the delay, since its first description, the etiopathogenesis of this affection stays unclear. Among the risk factors there are: intense physical activity, pregnancy, trauma, surgery (breast reconstruction, breast biopsy, oncology surgery, etc.), various diseases (neoplasia, breast infection, inflammatory process) and thrombophilia [5 , 6, 8, 9]. For the first patient, the likely aetiology was a direct trauma to the breast. Another likely risk factor is breast neoplasia, even if the cause and effect link has not yet been clearly etablished yet. One study found a rate of 12.7% of MD with no obvious cause occurring in the field of neoplasia. Another study by Hasegawa and Okita found a case of MD occurring on the left breast after a right breast neoplasia as it was the case for our second patient.
However, for this specific case, the aetiology found was a direct trauma resulting from the placement of an intravenous catheter for chemotherapy [5]. For this second case, this aetiology could also be retained because the left mastectomy and axillary dissection was done 15 days ago, with venous approach on the right.. The 2005 Lhoeststudy of the complications of breast surgery found a frequency of 1.58% of MD without specificity in relation to the type of surgery with patients who developed the symptomatology 10 to 15 days after the intervention as it was the case for our patient [3, 10].
The clinical symptomatology found in our two patients was similar to what was described in the literature [4]. We discovered a cord with the form of a groove, a rectilinear gutter or, on the contrary, a linear relief better visible during breast elevation or arm abduction.
The topography is variable depending on the venous involvement [12] (Figure 3)
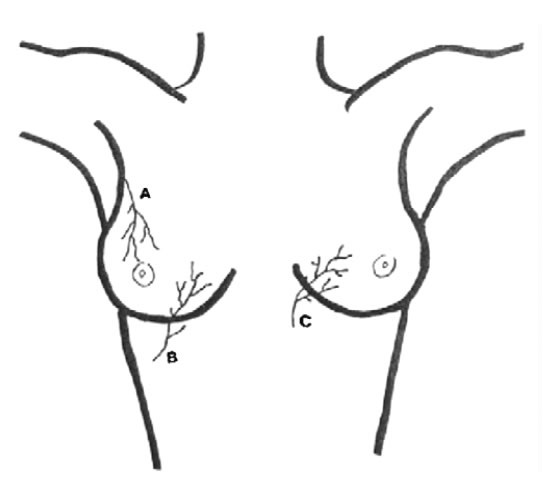
Figure 3. Superficial veins of the anterolateral chest wall
A: Lateral thoracic avein
B: Thoraco epigastric vein
C: Superior epigastric vein
1. If the lateral thoracic vein is thrombosed, there is an oblique cord in the SEQ running up and out towards the axillary hollow along the outer edge of the pectoralis major;
2. If the thoraco-epigastric vein is affected, the cord located in the lower quadrant takes a direction rather down and out;
3. Finally, if it is the upper epigastric vein, it takes a direction from the infero-internal quadrant below and inside.
The size of the cord is variable, from a few millimeters to several centimeters; it extends over 20 to 30 cm sometimes less and can touch the upper limb by contiguity. In our two patients, the clinical examination was sufficient to recognize the pathology, the ultrasound associated with venous Doppler confirmed the diagnosis. Several authors believe that ultrasound associated to venous doppler is currently the gold standard for the diagnostis. We found the usual signs of venous thrombosis (non-compressibility of the vein under the probe and hypoechogenicendoluminal image) [1,4,11]. However, since the link with breast neoplasia is still not clearly established; we will recommend a mammogram even an MRI in the follow-up, especially in cases where no risk factors have been found. For our first patient, we did a breast MRI and a mammogram to find out an etiology to the increase of breast volume observed after the trauma.
Concerning care, wherever the MD is located, it is necessary to treat the cause or the predisposing factors if they are found to promote healing and avoid recurrence. Generally it is recommended either to abstain from therapy, than a simple analgesic or anti-inflammatory treatment, especially in cases where the pain is very significant. In a study carried out by Shirah which tested two therapeutic modalities namely a treatment based on NSAIDs by oral and local way, he found that the local way traetment was more effective because of its speed of action [1]. Some authors have reported the efficiency of an anticoagulant therapy in the acute phase, but this remains controversial [1,4].
Our first patient had spontaneous recovery without treatment. For the second patient, due to the pain and the stress caused by contralateral breast neoplasia, treatment with oral NSAIDs was started, with symptoms disappearing in less than 10 days. This further confirms the benign nature of this affection.
Conclusion
Mondor’sDisease (MD) is a rare and benign affection. It is a venous vascular pathology most often affecting the vessels of the anterolateral chest wall. Its real incidence and its etiopathogenesis are still unclear due to the few cases described in the literature. The clinical examination is generally sufficient to make the diagnosis. It is a pathology which is most often spontaneously resolved within a few days even in the absence of treatment.
References
- Shirah BH, Shirah HA, Alonazie WS(2017) The Effectiveness of Diclofenac Sodium in the Treatment of Mondor’s Disease of the Breast: The Topical Patch Compared to the Oral Capsules. The Breast Journal 23 : 395-400.[crossref]
- Zidani H, Foughali M, Laroche JP (2010) Superficial venous thrombosis of the penis: penile Mondor’s disease? A case report and literature review. Journal des Maladies Vasculaires35: 352-354.[crossref]
- Lhoest F, Grandjean FX, Heymans O (2005)Mondor’s disease: a complication of breast surgery. Annals of cosmetic plastic surgery50: 197-201.
- Quéhé P, Saliou AH, Guias B, Bressollette L (2009) Mondor’s disease in 3 cases and review of the literature. Journal of vascular diseases34 : 54-60.[crossref]
- Olarinoye-Akorede SA, Silas BT (2017) Mondor’s disease of the breast in a Nigerian woman previously treated for invasive ductal carcinoma in the contralateral breast: A case report. Niger J Clin Pract20:1040-1043.[crossref]
- Amano M, Shimizu T (2018) Mondor’s disease: A review of the literature. Intern Med 57: 2607-2612. [crossref]
- Pasta V, D’Orazi V, Sottile D, Del Vecchio L, Panunzi A et al (2015) Breast Mondor’s disease: Diagnosis and management of six new cases of this underestimated pathology. Phlebology30: 564-568.[crossref]
- Ouattara A, Paré AK, Kaboré AF, Yaméogo C, Botcho G et al. (2019) Subcutaneous Dorsal Penile Vein Thrombosis or Penile Mondor’s Disease: A Case Report and Literature Review. Case Reports in Urology. [crossref]
- Wong SN, Lai KL, Chan PF, Chao DVK (2017) Mondor’s disease:sclerosing thrombophlebitis. Hong Kong Med J23: 311-312.
- Goldman A, Wollina U.Mondor’s (2018) Disease after Aesthetic Breast Surgery: A Case Series and Literature Review. J Ctan Aesthet Surg11: 132-135.[crossref]
- Rountree KM, Barazi H, Aulick NF. Mondor Disease. [Updated 2019 May 19]. In: StatPearls [Internet]. Treasure Island (FL):StatPearls publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538282/.