Introduction
Paraganglioma of the urinary bladder is rarely encountered and its biological behavior is uncertain. Paragangliomas are extra-adrenal neoplasms of the neural crest derivation, and if hormonally active, they are termed pheochomocytoma. They account for less than 0.05 % of all bladder tumors and less than 1 % of all pheochromocytomas [1]. In the genitourinary tract, the urinary bladder is the most common site (79.2 %), followed by the urethra (12.7 %), pelvis (4.9 %), and ureter (3.2 %) [2,3]. Haematuria and intermittent hypertension during micturition are among the usual clinical signs along with generalised symptoms due to raised catecholamines such as headache, blurred vision, heart palpitation and flushing. Furthermore, the consequences of hypertension itself may muddle the initial diagnostic picture of these patients. Patients often seek medical attention only when their hypertension has become so advanced as to cause syncope, retinopathy or intracranial haemorrhage. In addition, symptoms and signs of urethral obstruction may occur when the tumour is within the vicinity of the urethral opening(4).However, 27 % of pheochromocytoma of the urinary bladder do not feature any hormonal activity [3]. The pheochromocytoma of the bladder was first described by Zimmermann in 1953 [5], and a little more than 100 cases have been spotted since then [1].
Treatment strategies for these tumours are not well-defined because of their rare incidence. We present a rare case of paraganglioma of the urinary bladder where a partial cystectomy was performed.
Case report
12yr old boy presented with history of episodic severe headache for 2 months duration; severe, holocranial associated with vomiting episodes. Headache was often accompanied with diaphoresis, anxiety and nervousness. He also had history of left retinal detachment one year back .On evaluation he was found to be hypertensive, BP – 200/170 mm Hg. There was no history of any familial disorder (MEN syndrome) or family h/o hypertension. Biochemical assessment revealed an elevated 24-hour normetanehrine of 3863/24 hours (<600).Initial localization of the paraganglioma was through contrast enhanced computed tomography (CT) of the abdomen and pelvis which revealed intensely enhancing lesion (4.5 x 2.7 cm) at superior border of urinary bladder with loss of fat planes; two more similar lesions (? Lymph nodes) were present in peri-vesicle locations along iliac vessels. GA 68 – DOTANOC PET scan confirmed disease limited to urinary bladder and Bilateral iliac lymph nodes. After an extensive effort to control his blood pressure with prazosin and Metoprolol, excision of the tumour along with pelvic lymph node excision was performed under general anaesthesia. Prior cystoscopic examination extrinsic compression at dome of bladder with increased vascularity. Bilateral ureteric catheterisation (5 Fr) was performed in view of identification of ureters during pelvic lymph node dissection. Partial cystectomy with pelvic lymph nodal dissection was successfully performed with minimal fluctuation of his blood pressure. The post-operative period was uneventful and histopathological examination confirmed the diagnosis of pheochromocytoma of the urinary bladder. All anti-hypertensive medications were discontinued immediately after the operation. Micturating Cysto-Uretherogram (MCU) done on 10th post-operative day reveal satisfactory bladder capacity (250 ml) with no leak or residual volume. Histopathological report was malignant paraganglioma with lymph node metastasis. Two external iliac lymph nodes were positive for metastatic deposits.
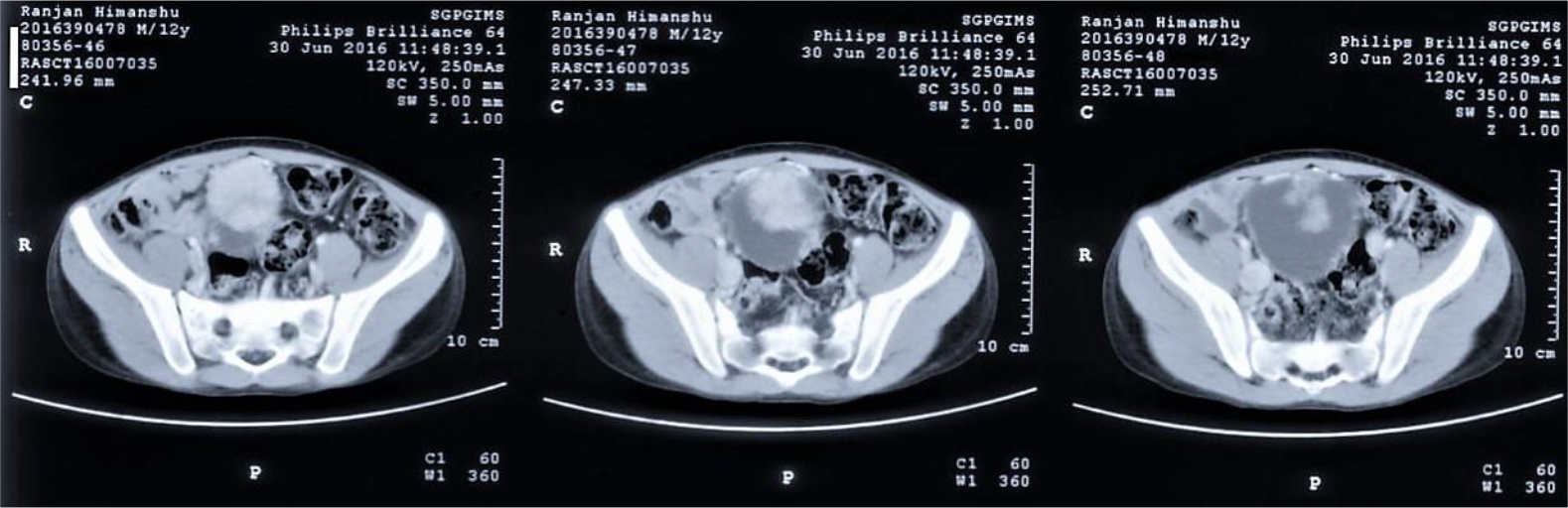
Image 1 – CT scan images showing transverse sections at level of urinary bladder showing enhancing mass lesion(4.5cm x 2.7 cm) at superior border of Urinary border.
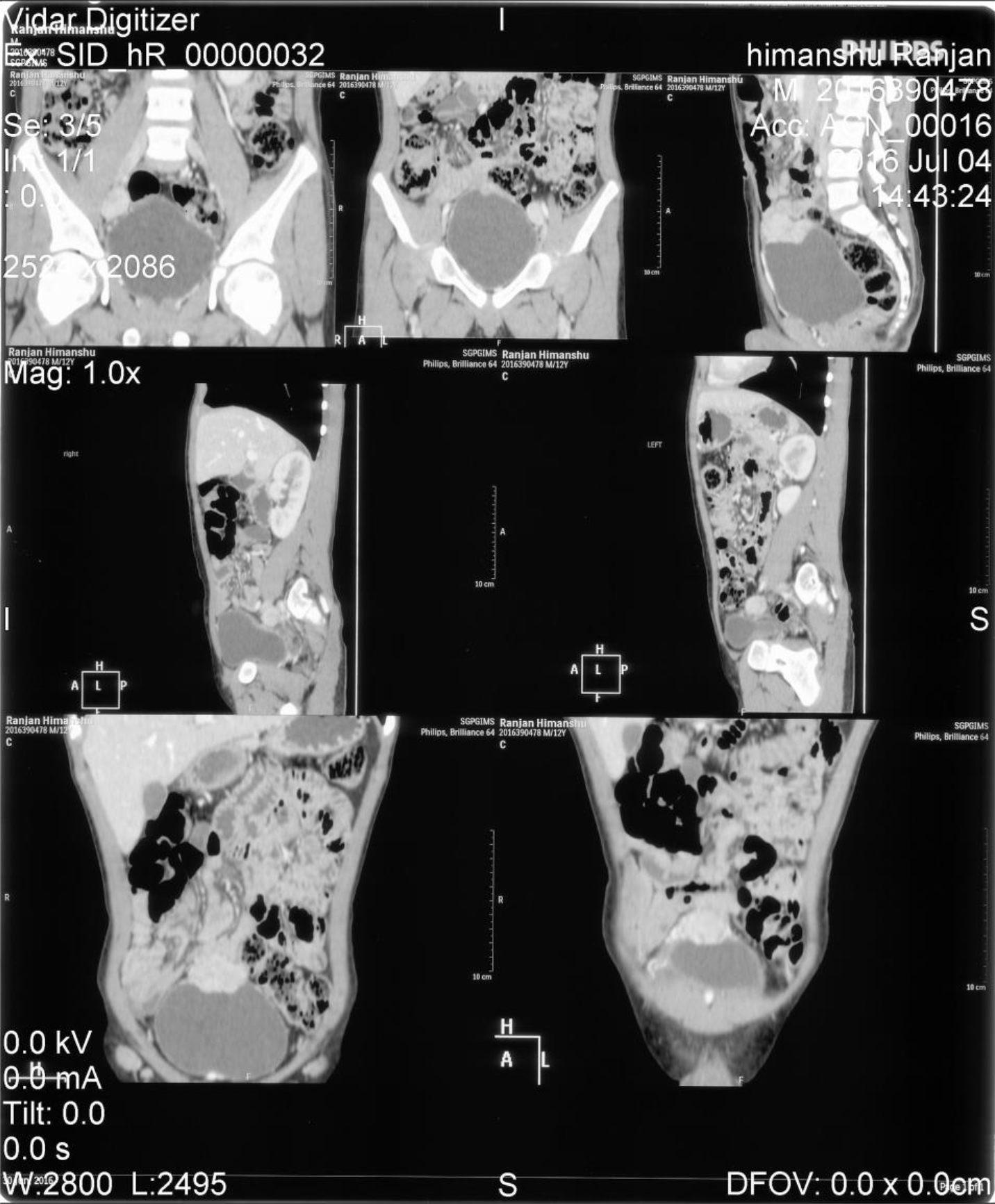
Image 2 – CT scan showing coronal and saggital images of lesion at superior border of urinary bladder along with two similarly enhancxinglesions (lymph nodes) in perivesical location.

Image 3 – Gallium – 68 DOTANOC PET scan showing somatostatin expressing urinary bladder mass lesion with bilateral external iliac lymph nodal involvement.

Image 4 – Surgical specimen showing Bladder paraganglioma(5x5xcm,inner surface seen) and bilateral external iliac lymph node ( about 3x 2cm , 3 in number, largest – 3×2 cm, firm).
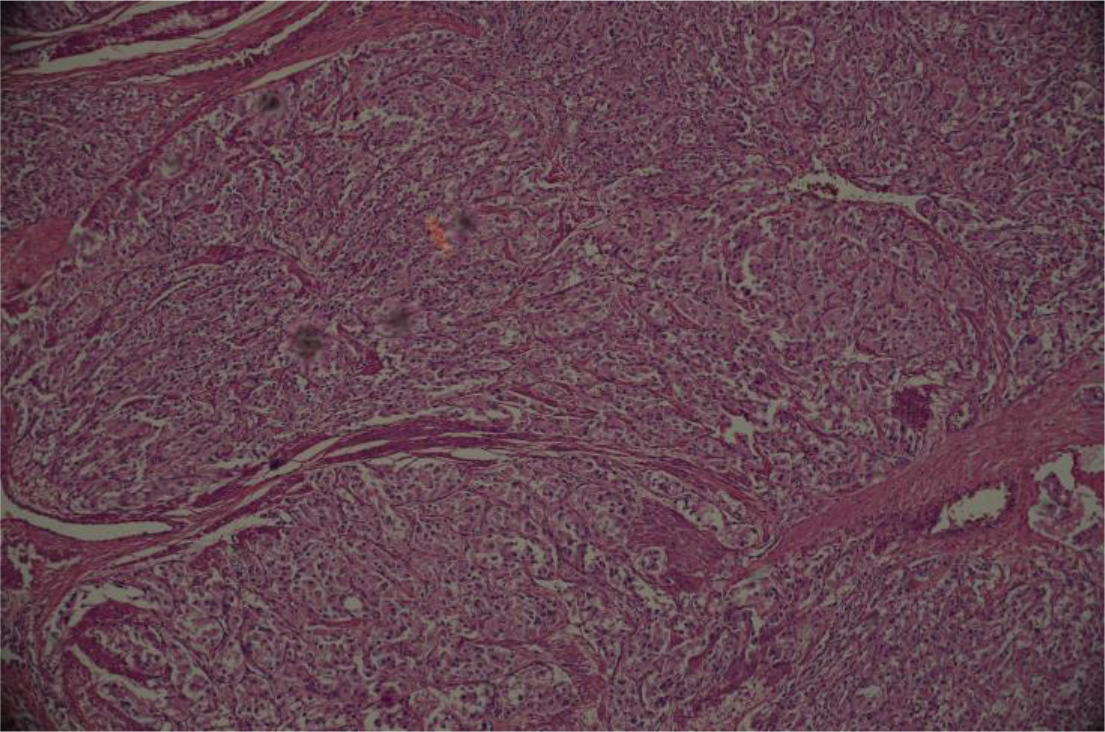
Image 5 – Low power view of tumor. Tumor shows nests of cuboidal cells separated by vascularised fibrous septa. This pattern of arrangement of tumor cells is k/a Zellballen.
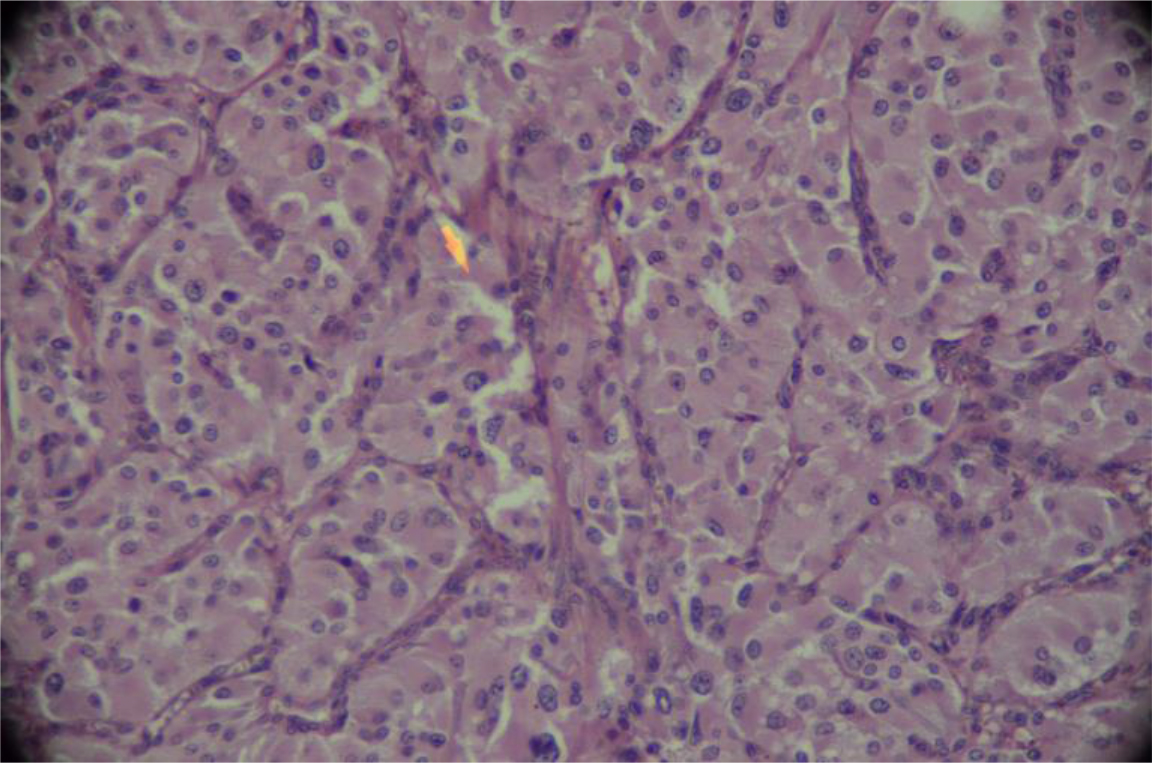
Image 6 – High power view Shows zellballen formation and tumor cells with moderate amount of cytoplasm.
Discussion
The commonest bladder tumor in children is rhabdomyosarcoma. (Huppmann AR, Pawel BR. Polyps and masses of the pediatric urinary bladder: a 21-year pathology review. Pediatr Dev Pathol. 2011; 14(6): 438-44.) Paragangliomas of the urinary bladder are rare tumors that can present at any age (range 11–84 years) with a mean age of 45 years and with slight female sex predilection [1]. In the pediatric population they are extremely rare, with just over 12 cases reported in the literature [6]. The commonest site within the bladder is the trigone and the posterior wall [8].The lateral wall has also been cited as a common site [7].As many as 50% of the paragangliomas are hereditary and may be associated with familial paraganglioma, neurofibromatosis type 1, von Hippel- Lindau disease, and the Carney triad [9].Histologically, they are characterized by cells arranged in discrete nests separated by a prominent sinusoidal network. Malignant paraganglioma of the urinary bladder constitutes 10% of all the bladder paragangliomas [10, 12]. No reliable histologic criteria exist to distinguish malignant from benign neoplasms. Differentiation from benign bladder paragangliomas is based on local invasion, lymph node involvement, or distant metastases [10]. Approximately 30 malignant cases have been reported so far in the literature [11].
Suspected cases of paraganglioma should first be investigated by measuring the levels of catecholamine and metabolites such as metanephrine and vanillylmandelic acid secretion in either blood or urine. However, in cases of nonfunctional paragangliomas, the metabolites may be normal. Imaging can be used to evaluate the primary tumor as well as metastatic lesions. MR imaging is highly useful for imaging extra-adrenal pheochromocytomas. It may reliably differentiate pheochromocytoma from the more common epithelial neoplasms of the bladder which are characteristically poorly enhancing. On MR imaging paragangliomas are typically more hyper intense on both T1- and T2-weighted images.[13]
Bladder Pheochromocytomas is mainly treated by surgical excision. Preoperative catecholamine blockade is necessary for functional tumors. Metastatic or recurrent tumors are treated with palliative therapy [1]. Cystoscopic examination prior to the excision helps to delineate the exact location of the lesion, especially with regard to the depth of invasion and the involvement of the ureters. Biopsy should be avoided. On cystoscopy, pheochromocytomas appear as solid reddish brown granulated and lobulated lesions with or without ulceration [14]. Since the sympathetic plexus of the bladder is scattered between all the layers of the bladder, transurethral resection alone is associated with a high rate of recurrence and partial cystectomy is the standard of care where bladder can be preserved or else a total cystectomy is done. Open approach is preferred [14, 15, 16] although laparoscopic approach, as reported by Kozlowski et al, has recently been shown to be feasible [17].
References
- Beilan JA, Lawton A, Hajdenberg J and Rosser CJ (2013) Pheochromocytoma of the urinary bladder: a systematic review of the contemporary literature. BMC Urol 13: 22.
- Das S and Lowe P (1980) Malignant pheochromocytoma of the bladder. J Urol 123: 282–4.
- Hanji AM, Rohan VS, Patel JJ and Tankshali RA (2012) Pheochromocytoma of the urinary bladder: a rare cause of severe hypertension. Saudi J Kidney Dis Transpl 23: 813–6.
- Bonacrzu Kazzi G. Asymptomatic bladder pheochromocytoma in a 7-year-old boy. J. Paediatr Child Health 2001; 37: 600–2.
- Zimmerman I J, Biron RE and MacMahon HE (1953) Pheochromocytoma of the urinary bladder. N Engl J Med 249: 25–6.
- Bohn OL, Pardo-Castillo E, Fuertes-Camilo M, Rios-Luna NP, Martinez A and Sanchez-Sosa S. Urinary bladder paraganglioma in childhood: a case report and review of the literature. Pediatr Dev Pathol 2011; 14: 327–32
- Cheng L, Leibovich BC, and Cheville JC. Paraganglioma of the urinary bladder: can biologic potential be predicted? Cancer. 2000; 88: 844–52.
- Messing EM. Urothelial tumors of the bladder. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW and Peters CA. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders; 2007. p. 2407.
- Young WF Jr. Paragangliomas: clinical overview. Ann N Y Acad Sci. 2006; 1073: 21–9.
- Ka iri-Vassilatou E, Argeitis J, Nika H, Grapsa D, Smyrniotis V and Kondi-Pafiti A. Malignant paraganglioma of the urinary bladder in a 44-year-oldfemale: Clinicopathological and immunohistochemical study of a rare entity and literature review. Eur J Gynaecol Oncol 2007; 28: 149–51.
- Palla AR, Hogan T and Singh S. Malignant paraganglioma of the urinary bladder in a 45-year-old woman. Clin Adv Hematol Oncol 2012; 10: 836–9.
- Ansari MS, Goel A, Goel S, Durairajan LN and Seth A. Malignant paraganglioma of the urinary bladder. A case report. Int Urol Nephrol 2001; 33: 343–5.
- Loveys FW, Pushpanathan C and Jackman S. Urinary Bladder Paraganglioma: AIRP Best Cases in Radiologic-Pathologic Correlation. Radiographics. 2015; 35(5): 1433–1438. doi: 10.1148/rg.2015140303
- Doran F, Varinli S and Bayazit Y. Pheochromocytoma of the urinary bladder. APMIS 2002; 110: 733–6.
- Young WF Jr. Paragangliomas: clinical overview. Ann N Y Acad Sci. 2006; 1073: 21–9.
- Dahm P and Gschwend JE. Malignant non-urothelial neoplasms of the urinary bladder: a review. Eur Urol. 2003; 44: 672–81.
- Klingler HC, Klingler PJ, Martin JK Jr, Smallridge RC, Smith SL and Hinder RA. Pheochromocytoma. Urology. 2001; s57: 1025–32.