DOI: 10.31038/SRR.2020313
Introduction
Most people accept that COVID-19 is very infectious which is why in the United Kingdom, it is recommended and accepted that individuals who have been in contact with those with proven clinical COVID-19 should isolate for 14 days. Similarly this is the basis of the quarantine rule-if an individual has been in contact with a proven clinical case travelling into the UK. It is assumed that the clinical infection will have shown by 14 days. This also assumes that infectivity is linear after close and significant contact, at least for 30 minutes.
However, measles has always been one of the most contagious diseases. In fact, to quantify this infectivity, if 100 susceptible people are in a room with someone who is infected, 90 of them are likely to become ill with measles. Further, if someone who has not had measles enters an elevator or other small space up to two hours after an infected person has left, they can still “catch” measles. There is no doubt that the COVID-19 virus affects children and adults. Unusually, the level of infectivity does not directly correlate with clinical symptoms, as an explanation for asymptomatic individuals. It is now generally accepted that infected individuals may be asymptomatic.
Some risk factors have been observed with COVID-19 deaths. These include much older age, diabetes mellitus, immune disorders, renal diseases, cancer, BAME individuals and even asthma. However an association, for example between diabetes and COVID-19 deaths does not mean that diabetes has a plausible way of exposing COVID-19 patients to COVID-19 deaths. In epidemiological parlance, association does not mean cause. The observations between the current risk factors and COVID-19 deaths are very tenuous because of the implausibility, except for much older age. It is a clinical curiosity that some individuals who have had classical clinical manifestations who do not need to attend a hospital might not show any evidence of IgG awareness subsequently. However, there are currently no reports of IgG antibody status in clinically proven cases.
SARS-CoV-2 infection is a major killer of adults, particularly older adults. So far it has killed 190,000 American adults and over 41,586 United Kingdom adults, and many more worldwide. So far there have only been 6 childhood deaths under the age of 16 years. What is so special about SARS-COV-2 infection that excessively affects the mortality of much older adults but does not seem to proportionately affect the mortality of children? This is a legitimate clinical curiosity. This Corona SARS-COV-2 virus, in the same class as Measles, Rubella, Polio and Mumps is a child’s virus but has not caused the havoc of measles, in childhood deaths. It is now widely accepted that SARS-CoV-2 infection does not cause massive mortality in children.
To assess the infectivity of SARS-COV-2, this investigative study sought to assess the infectivity potential between close family relations of those who have come in contact with COVID-19 virus using IgG assessments within members of families living together.
Hypothesis
SARS-V-2 infection is assumed to be very infectious. If so, we expect a high infection rate, identified with Anti-SARS CoV- 2 IgG antibodies. We explored this through family trees of IgG tests. The ultimate outcome is to assess whether members of a family living together will get the infection from symptomatic or even from asymptomatic relatives.
Methods
We explored the results of Anti-SARS CoV-2 IgG antibodies in families to assess the likelihood of multiple members of a family having a positive Anti-SARS CoV-2 IgG antibodies. A linear relationship of infectivity is defined for our purposes as positive results between family members living together. The assumption is that if COVID-19 is as highly infectious and transmitted with causal contact, say on a flight or contact within a household, various members of a family will demonstrate evidence of contact through positive Anti-SARS CoV-2 IgG antibodies (Figure 1).
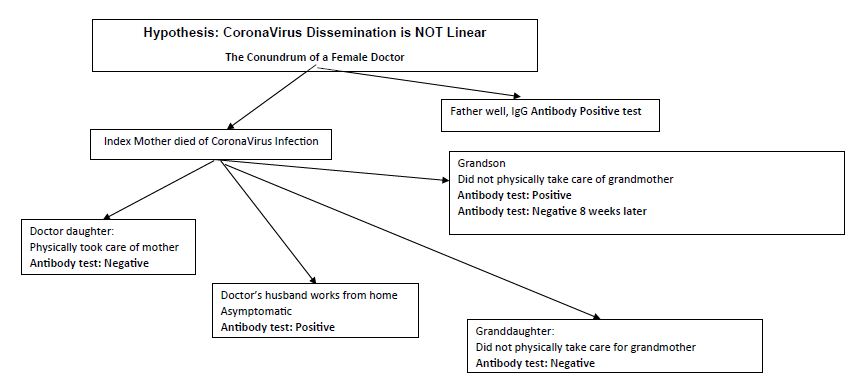
Figure 1: Clinical and IgG status.
Results
In Table 1, we present the results of the assessment of linear relationships between family members based on IgG results of contact with COVID-19. Of the 39 reported families, there were 11 linear relationships (28% infection rate) where more than one member of a family have both shown IgG evidence of contact with SARS CoV-2 or COVID-19 infection. In Table 2, we summarise that 11/39 (28%) families showed more than one person in a family with positive IgG antibodies. In 28/39 families (72%) there was no evidence of linearity. The odds of linearity was similar for both groups [Odds Ratio = 1].
Table 1: Report of IgG Status in Families who wished to be tested for contact with SARS-Covid 2 IgG Antibodies.
|
Family |
Grandmother | Grandfather | Mother | Father | Son 1 | Son 2 | Daughter 1 | Daughter 2 |
Comment |
| 1 | Died of Covid-19 | IgG positive | IgG Negative | IgG positive | IgG positive | n/a | ?? | IgG Negative |
Not linear |
|
2 |
n/a | n/a | IgG Negative | IgG positive | IgG positive | IgG Negative | IgG Negative | n/a | Not linear |
|
3 |
n/a | n/a | IgG positive | IgG Negative | n/a | n/a | IgG Negative | n/a |
Not linear |
| 4 | n/a | n/a | IgG positive | IgG positive | n/a | n/a | IgG positive | n/a |
Linear |
|
5 |
n/a | n/a | IgG positive | IgG Negative | IgG positive | n/a | IgG Negative | n/a | Not linear |
| 6 | n/a | n/a | IgG positive | IgG positive | n/a | n/a | IgG positive | IgG positive |
Linear |
|
7 |
n/a | n/a | IgG positive | IgG positive | IgG positive | n/a | n/a | n/a | Linear |
| 8 | n/a | n/a | IgG positive | IgG positive | IgG positive | IgG positive | n/a | n/a |
Linear |
|
9 |
n/a | n/a | IgG Negative | IgG Negative | IgG Negative | IgG positive | IgG Negative | n/a | Not linear |
| 10 | n/a | n/a | IgG positive | IgG Negative | IgG Negative | n/a | IgG positive | IgG positive |
Not linear |
|
11 |
n/a | n/a | IgG positive | IgG positive | n/a | n/a | IgG Negative | IgG positive | Not linear, Nanny IgG negative |
| 12 | n/a | n/a | IgG Negative | IgG Negative | IgG Negative | n/a | IgG positive | n/a |
Not linear |
|
13 |
n/a | n/a | IgG positive | IgG Negative | n/a | n/a | n/a | n/a | Not linear |
| 14 | n/a | n/a | IgG Negative | IgG Negative | IgG positive | n/a | n/a | n/a |
Not linear |
|
15 |
n/a | n/a | IgG positive | IgG positive | n/a | n/a | n/a | n/a | Linear |
| 16 | n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a |
Not linear |
|
17 |
n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a | Not linear |
| 18 | n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a |
Not linear |
|
19 |
n/a | n/a | IgG positive | IgG Negative | IgG positive | n/a | IgG positive | n/a | Not linear |
| 20 | n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a |
Not linear |
|
21 |
n/a | n/a | IgG positive | IgG positive | n/a | n/a | n/a | n/a | Linear |
| 22 | n/a | n/a | IgG positive | IgG positive | n/a | n/a | n/a | n/a |
Linear |
|
23 |
n/a | n/a | IgG positive | Died of Covid | n/a | n/a | IgG positive | n/a | Linear |
| 24 | n/a | n/a | IgG positive
IgG Negative |
n/a | n/a | n/a | n/a | n/a |
Not linear |
|
25 |
n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a | Not linear |
| 26 | n/a | n/a | IgG Positive | n/a | n/a | n/a | IgG Negtive | n/a |
Not linear |
|
27 |
n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a | Not linear |
| 28 | n/a | n/a | IgG Negative | IgG positive | IgG Positive | IgG Negative | IgG Negative | n/a |
Not linear |
|
29 |
n/a | n/a | IgG Negative | n/a | n/a | IgG Positive | n/a | n/a | Not linear |
| 30 | n/a | n/a | IgG positive | IgG positive | n/a | n/a | n/a | n/a |
Linear |
|
31 |
n/a | n/a | n/a | IgG positive | IgG positive | n/a | IgG Negative | n/a | Not Linear |
| 32 | n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a |
Not linear |
|
33 |
n/a | n/a | IgG positive | IgG positive | n/a | n/a | IgG positive | n/a | Linear |
| 34 | n/a | n/a | IgG positive | IgG positive | n/a | n/a | IgG positive | n/a |
Linear |
|
35 |
n/a | n/a | IgG Negative | IgG positive | IgG Negative | n/a | IgG Negative | n/a | Not linear |
| 36 | n/a | n/a | IgG Negative | IgG positive | n/a | n/a | n/a | n/a |
Not linear |
|
37 |
n/a | n/a | IgG Negative | IgG Negative | IgG positive | IgG positive | n/a | n/a | Not linear |
| 38 | n/a | n/a | IgG positive | IgG positive | IgG Negative | n/a | n/a | n/a |
Not linear |
|
39 |
n/a | n/a | IgG positive | n/a | n/a | n/a | IgG Negative | n/a |
Not linear |
Note: n/a not applicable.
Table 2: Statistical summary of linear relationships.
|
Proportions |
Linearity | Non-Linearity |
Odds Ratio |
|
11/39 (28%) |
28/39 (72%) |
1 |
Conclusion
In this family tree study, 28% of families showed evidence of a potential linear transfer of infection of COVID-19 to others in their household. Based on our definition of linearity, there is no significant evidence to suppose that prior contact with COVID-19 of a member of the family translates to a high linear infection in close contacts (Odds Ratio = 1.0). This is the first study that casts doubt on the assumed degree of infectivity of COVID-19. It is certainly not in the category of measles. There is one possible explanation, that IgG antibodies do not measure casual contact in this situation. It is also possible that IgG positive antibodies can sero-convert to IgG negative antibodies within short period of time. Certainly this was suggested in Wuhan [1] where people who had definite contact with clinical relatives with clinical COVID-19 patients yet they showed no serological evidence of contact with COVID-19.
References
- Lu X, Zhang L, Du H (2020) For the Chinese pediatric novel coronavirus study team. N Engl J Med 382: 17.