DOI: 10.31038/SRR.2020312
Abstract
Background: The pandemic pattern of COVID-19 in some countries appears to have started a deceleration stage. It is recommended to restart as soon as the situation is under control and some tools exist for interpreting the ICU capacity under conditions of health system stress. However, there are no clear guidelines or a strategy to restart Bariatric and Metabolic (B&M) surgery.
Objective: To present a protocol proposal to assist surgeons in restarting elective B&M surgery after the outbreak.
Method: This document presents a recommended protocol based on experts’ opinions, reviews of small series and publications from previous different viral epidemic outbreaks.
Results: Priority is for patients who would benefit most from a B&M procedure with limited risk. Patients being eligible for surgery must be screened for COVID-19. Only patients with negative results will have surgery. Radiofrequency/electro thermal bipolar devices are recommended. A smoke evacuator machine with a closed-circuit system should be used. All patients must be treated as if they are suspected to be COVID-19 positive. Proper personal protective equipment should be applied. Post-operative follow-up consultations should be via telemedicine. The RT-PCR screening test should be repeated for legal documentation purposes and to make sure that the patient is COVID-19 free.
Conclusion: The resumption of elective B&M surgeries during deceleration stage of COVID-19 must be gradual and prudent. This scholarly protocol can be adjusted according to the regulations established by the local health departments and with the increased acquisition of new knowledge; there would be changes in the current recommendations.
Keywords
Covid-19 pandemic, Metabolic surgery, Sleeve gastrectomy, Bariatric and metabolic surgery
Introduction
The future and aftermath of the COVID-19 global pandemic is unknown but will be dependent on how the medical societies and governments react to the current situation. Many of the international health organizations and federations have combined efforts to fight against the COVID-19. European and American guidelines as well as IFSO recommendations have been issued and most elective surgeries were postponed, as a cautious measure to minimize the spread of the infection and to cope with the emerging scarcity of health care resources, particularly ventilators and other critical care equipment [1,2]. The American College of Surgeons (ACS) issued COVID-19 elective case triage guidelines for surgical care, including (B&M) surgery. The guidelines recommended delaying the elective cases, even for months [1].
The worldwide numbers of patients’ morbidity, mortality as well as the timelines to peak incidence are very inconsistent. The pandemic pattern in some countries appears to have started a deceleration stage. Epidemiology expertise across the globe expect to see a flattening of the COVID-19 infection curve. The virus is not expected to vanish suddenly, but more slowly through a transitional period.
This document presents a scholarly protocol for surgeons to assist them in restarting elective B&M surgery after the COVID-19 outbreak is on the decline and it is deemed safe to do so. It is recommended to restart as soon as the situation is under control. There should be few newly diagnosed cases and the hospitals do not receive a surge of COVID-19 patients. It will likely be variable between countries and even between B&M surgery programs within the same country. Surgeons should be aware of the regional health care status and the hospital beds capacity. Some tools exist for interpreting the Intensive Care Unit (ICU) beds capacity under conditions of health system stress. Criticon was designed by a UK critical care network to interpret the ICU capacity during the influenza pandemic and remains in modified use [3]. Also, healthcare workers in the US launched an interactive data platform that allows people to analyze and monitor US hospital beds capacity during the COVID-19 outbreak.
Discussion
The benefits to restart performing elective B&M surgeries
Bariatric surgeons and patients eagerly look forward to restarting the elective surgeries. There are indisputable benefits of early surgical intervention for patients with morbid obesity. Delaying elective B&M surgery may adversely affect the benefits of surgery for achieving a resolution of obesity and its complications.
There is a worldwide concern about the severity of COVID-19 when contracted by patients with morbid obesity. The history of previous pandemics of different viral influenza-like illnesses revealed a strong association between morbid obesity and the severity of the illness and hospital and ICU admissions [4,5]. Additionally, it has been reported anecdotally by a number of surgeons that patients who have had successful bariatric surgery that resulted in significant weight loss and the resolution of co-morbid conditions such as hypertension and diabetes, have been able to overcome the COVID-19 disease and its pulmonary complications.
The elective B&M surgeries
According to ACS guidelines, the elective B&M surgeries are primary gastric bypass, sleeve gastrectomy, duodenal switch, gastric banding, revisions or conversions for weight gain [1] and endoscopic bariatric procedures. Prioritization of the elective list aims to avoid a bad outcome if COVID-19 infection occurs:
• Patients with controlled comorbidity but who may deteriorate over time.
• Semi-elective urgent cases: Revisional cases (for dysphagia, severe Gastro esophageal Reflux Disease (GERD), dehydration/malnutrition, slipped band, gastric band erosion, anastomotic strictures at risk for aspiration), patients pending surgery requiring pre-operative weight loss (transplant, etc..), endoscopic procedures: balloon removal [1].
A hidden or acquired infection during the perioperative period could be fatal. A recent study reported that out of four gastric bypass surgery patients who developed COVID-19, two (50%) were admitted to the ICU, although all survived [6]. A Careful risk/benefit assessment in collaboration with the anesthesiologists would be beneficial. There should be a priority to identify patients who will benefit most from B&M surgery while keeping the risks as low as possible. The surgeons must rely on their clinical sense, realize their surgical capabilities, and consider the available facilities.
Eligibility
• Asymptomatic patients (no flu-like symptoms, shortness of breath, fever, and/or GI symptoms)
• No history of COVID-19 positivity
• Age: 20 – 50 years
• BMI ≤ 50 kg/m2
• No co-morbidities: (i.e., Diabetes, Hypertension, Cardiac diseases)
• Controlled comorbidities that may deteriorate over time
• No Pulmonary diseases: (i.e., OSA, Asthma, Respiratory diseases)
• Non-smokers.
Hospital Course
This document targets hospitals under the non COVID-19 category. Specialized B&M surgery centers are preferred. We recommend gradual restarting and only performing1-2 cases per day. Hospital admission on the same day of surgery minimizes the hospital stay. As many pre-operative medical consultations should be via telemedicine and video phone calls as possible. The surgical consent should explain that the patients are at an increased risk of acquiring a COVID-19 infection during their hospital course. Patients should not allowed to be accompanied by relatives/co-patients during the hospital course and must agree on self-quarantine post-operatively for a minimum of 14 days (Figure 1).
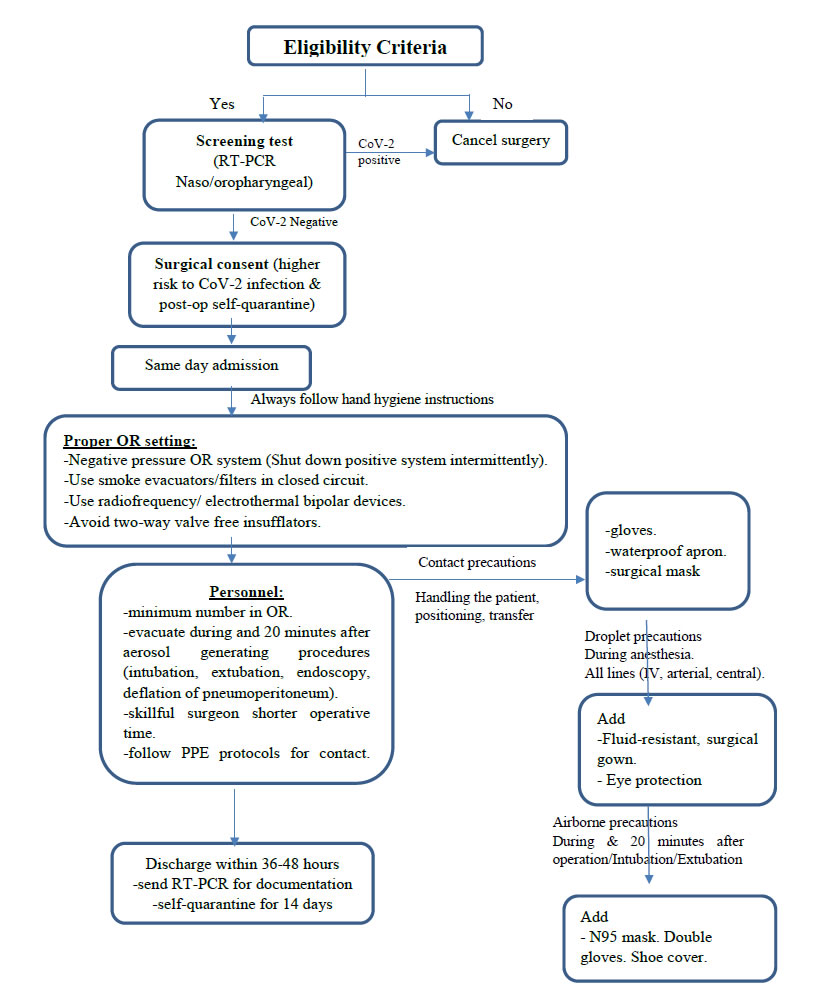
Figure 1. Protocol to restart performing elective bariatric and metabolic surgery after the peak of the COVID-19 pandemic.
Screening Test: (What and When)
Patients being considered for elective B&M surgery must be screened for COVID-19, twenty-four hours before the admission. Only patients with negative results will have surgery. Baseline screening is medically and legally essential. The virus RNA (SARS-CoV-2 RNA) is detected by Reverse-Transcription Polymerase Chain Reaction (RT- PCR). Authors from China reported the highest sensitivity rate of viral RNA tests was from bronchoalveolar lavage, followed by sputum [7]. Patients being considered for B&M surgery are asymptomatic and may not be able to produce sputum. A nasopharyngeal swab test would also be of benefit. A nasopharyngeal swab is more sensitive than an oropharyngeal one [7]. RT-PCR reports a false negative result in up to 30% of cases [7]. Both the RT-PCR and the antibodies serology tests are recommended for more accurate results. The World Health Organization assumes there is no evidence that COVID-19 antibodies protect from potential re-infection. A positive serology test excludes the patient from surgery during this transitional period. In case only one test is feasible, the RT-PCR is mandatory. The serology tests detect antibodies which are generated in blood a week or two after exposure to the virus, at which time the virus should have been cleared from the system.
Radiological screening: chest ultrasound is a highly sensitive tool in diagnosing the early COVID-19 patients. It is a less aggressive alternative without subjecting the patients to the high radiation exposure of a CT- chest or even a plain chest x-ray [8]. Some authors suggested that the lung characteristics of patients with COVID-19 are ideal for imaging with ultrasound. In addition, in contrast to the CT device, the ultrasound device is portable, easier to sterilize and decreases the risk of cross-infection. The ultrasound device also minimizes the number of personnel exposed to the risk of cross- infection [9,10].
OR settings and Operative technique
The current ventilator systems found in almost all Operating Rooms (OR) are positive pressure systems. However, negative pressure systems decrease the risk of infection [11]. It is important to operate in a negative pressure OR when available. During this pandemic, some hospitals solved this issue of OR ventilation to avoid or minimize the positive pressure by shutting down the ventilatory system intermittently during operations for approximately 60 minutes each time.
The transmission of aerosols and droplets is very risky. They remain in the OR environment for up to 20 minutes after the procedure [12]. Staff who is not essential for the procedure should leave the OR during surgery and not return until 20 minutes after an Aerosol Generating Procedure (AGP) is completed. AGPs include endotracheal intubation, gastrointestinal endoscopy, and the evacuation of pneumoperitoneum and aspiration of body fluids during laparoscopic procedures.
Elective B&M surgeries are AGPs and generate a large amount of smoke. Up to our knowledge, there is no evidence of the presence of SARS-CoV-2 in the air of the abdominal cavity (laparoscopic pneumoperitoneum). However, small incisions and setting the intraperitoneal pressure to the minimum effective for safe surgery (10-12 mmHg), or even less is advised to avoid escaping of CO2. The surgical smoke produced during laparoscopic surgery is composed of 5% (cellular debris, aerosols, plume, chemicals, viruses and bacteria) and 95% steam or water [13]. Studies reported that the smoke produced from radiofrequency/electrocautery devices is less harmful [14,15]. The surgical plume production from an ultrasonic scalpel was in larger quantities and contained larger cellular debris when compared with that from electro cautery [13]. The plume produced by Sonicision obstructed 4% of the laparoscopic field whereas the ACE generated plume obstructed 25% [16]. We recommend using frequency/ electrothermal bipolar devices (e.g., LigaSure (LS; Covidien, Mansfield, MA), and Enseal G2 (ES; Ethicon Endo surgery), and not the ultrasonic coagulating devices.
Nevertheless, the preference of using radiofrequency energy device versus ultrasonic remains a scientific controversy. If an electrothermal device is used, a smoke evacuator machine must be used or connect the insufflation system to a filter. It minimizes the possible risk of infection through aerosolization [11]. Available commercial smoke evacuator options include: the Medtronic RapidVac™, Stryker Pneumo Clear, ConMed Airseal®, MEGADYNE™ and Valley lab™ Smoke Evacuators. The smoke evacuation systems in a closed-circuit are highly recommended in case of specimen removal and during Co2 extraction at the end of the procedure. In certain commonly used insufflator systems (ConMed Airseal®), there is a modality with criteria of stabilizing the intra-peritoneal pressure. The surgeons should not use this modality, it creates significant leakage and escape of CO2 which may increase the risk of infection [17]. In the setting of limited financial resources, surgeons may create a simple, very low-cost filtration system from available components in the operating room. Mintz and his colleagues utilized the standard electrostatic filter used in the ventilation machines for this purpose [18]. Surgeon competency is crucial. Only experienced surgeons should be operating in this time. It is well-known that the more skillful and experienced the surgeon is, the faster the procedure is performed, leading to a shorter operative time and less exposure to the aerosol.
Personal Protective Equipment (PPE)
Though the patient will be COVID-19 negative, 30% of the tests give false negative results. Accordingly, during this delicate transitional period, all patients must be treated as if they are suspected to be COVID-19 positive. Proper PPE should be applied. This will protect the medical staff and the patient from the risk of transmitting infection. A minimum number of surgeons, nurses and anesthetists should be present in the OR. The staff must follow all hand hygiene instructions at all times and follow the contact, airborne and droplet precautions (Table 1) explains the dress code of the medical staff in the OR during each step of the operation [19]. Studies have proven that there is no difference between N95 masks and powered air purifying respirators in protection against aerosols and droplets [17]. All OR personnel should always wear gloves. No trainees or observers should be allowed in the OR.
|
Table 1: Recommended personal protective equipment during elective bariatric and metabolic surgery after the peak of COVID-19 pandemic. |
||
| Precautions |
When to Apply |
What to Wear |
|
Contact |
Handling the patient, positioning, transfer from and to OR room, etc… |
(A); Gloves, waterproof apron and fluid resistant surgical mask |
|
Droplet |
During anesthesia. All lines (IV, arterial, central). During non AGP. |
(B); Consider (A) plus -Fluid-resistant, surgical gown. – Eye protection (face shield, goggles, etc.) |
|
Airborne |
Intubation/Extubation. During the elective B&M surgery (AGP). 20 minutes after the procedure (AGP). |
Consider (B) plus -N95 mask. -Double gloves. -Shoe cover. |
AGP: Aerosol Generating Procedure.
Post-Operative Course
All protective contact precautions should be applied during the patient’s hospital stay. The patient should be discharged as soon as possible. We recommend 36-48 hours (or less) of hospital stay. The RT-PCR screening test should be repeated for legal documentation purposes and to make sure that the patient is COVID-19 free when he/she leaves the hospital. All post-operative follow-up consultations should be via telemedicine and video phone calls. Some hospitals created a service of home delivery of medications to reduce the numbers of unnecessary hospital visits.
The first few weeks post B&M surgery are critical. Surgery may not only cause immediate impairment of the immune function, but also induces early systemic inflammatory response and more severe course in case of COVID-19 [20]. Additionally, the rapid loss of weight following bariatric surgery alter the patients’ immune system and may lead to the development of subclinical underlying immune disorders [21]. Therefore, a self-quarantine is recommended for a minimum of 14 days post- operatively. However, a period of up to 1 month is advisable.
Limitations
Data related to the subject of COVID-19 and elective surgery is limited. Most of the included studies in this protocol are based on experts’ opinions, reports of small series and publications from previous different viral epidemic outbreaks. It is possible that, with the passage of time and the increased acquisition of new knowledge, there would be changes in the current recommendations.
Conclusion
The resumption of elective B&M surgeries during the deceleration stage of COVID-19 is a delicate process, that must be gradual and prudent. There should be a priority for patients who would benefit most from a B&M procedure. The use of smoke evacuation machines is essential. The preference of using radiofrequency energy device versus ultrasonic remains controversial. This scholarly protocol can be adjusted according to the regulations established by the local health departments and available facilities. This paper is intended only as a recommendation to professionals and can in no way be used as an argument for possible legal claims.
Acknowledgement
The authors acknowledge Dr. Rossella Palma for her great help in preparation for this subject.
Disclosures
Drs. Luigi Angrisani, Nesreen Khidir, Juan Pujol Rafols, Michel Suter, Nicola Di Lorenzo, Ashraf Haddad, Miguel F Herrera and Lilian Kow have nothing to disclose.
Dr. Philippe Topart received teaching honoraria from Medtronic and Olympus, grant support from Ethicon and Leo pharmaceuticals.
Prof. Scott Shikora is the Editor-in Chief of Obesity Surgery.
References
- COVID-19: Elective Case Triage Guidelines for Surgical Care. Available at https://www.facs.org/covid-19/clinical-guidance/elective-case/metabolic-bariatric
- Yang W, Wang C, Shikora S. et al. Recommendations for Metabolic and Bariatric Surgery During the COVID-19 Pandemic from IFSO. OBES SURG (2020). https://doi.org/10.1007/s11695-020-04578-1[Crossref]
- Criticon designed by Critical Care Network-North West London. Available at https://www.londonccn.nhs.uk/managing-the-unit/capacity-escalation/critcon/
- Moser JS, Galindo-Fraga A, Ortiz-Hernández AA, et al. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir Viruses. 2019;13(1):3–9. doi:10.1111/irv.12618[Crossref]
- Simonnet A, Chetboun M, Poissy J et. Al. High prevalence of obesity in severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) requiring invasive mechanical ventilation. Obesity (Silver Spring). 2020 Apr 9. doi: 10.1002/oby.22831.
- Aminian A, Kermansaravi M, Azizi S, et al. Bariatric Surgical Practice During the Initial Phase of COVID-19 Outbreak [published online ahead of print, 2020 Apr 20]. Obes Surg. 2020;1‐4. doi:10.1007/s11695-020-04617-x[Crossref]
- Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. Published online March 11, 2020. doi:10.1001/jama.2020.3786.[Crossref]
- PoggialiE ,Dacrema A, Bastoni D. Et.al Can Lung US Help Critical Care Clinicians in the Early Diagnosis of Novel Coronavirus (COVID-19) Pneumonia? Radiology. Mar 13 2020https://doi.org/10.1148/radiol.2020200847[Crossref]
- Huang, Y, Wang S, Liu Y et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19). SSRN 2020. Epub 28 February. doi.org/10.2139/ssrn.3544750 (accessed 06/04/2020).
- Soldati G, Smargiassi A, Inchingolo R, et al. Is there a role for lung ultrasound during the COVID-19 pandemic? Journal of Ultrasound in Medicine 2020. Epub 20 March. doi.org/10.1002/jum.15284
- Chow TT, Yang XY. Ventilation performance in operating theatres against airborne infection: review of research activities and practical guidance. Journal of Hospital Infection. 2004;56(2):85-92.[Crossref]
- Brat GA, Hersey SP, Chhabra K, Gupta A, Scott J. Protecting Surgical Teams During the COVID-19 Outbreak: A Narrative Review and Clinical Considerations. Annals of surgery. (March 2020) available at https://journals.lww.com/annalsofsurgery/Documents/COVID%20Surgery_VF.pdf[Crossref]
- Liu Y, Song Y, Hu X, Yan L, Zhu X. Awareness of surgical smoke hazards and enhancement of surgical smoke prevention among the gynecologists. J Cancer. 2019;10(12):2788–2799. Published 2019 Jun 2. doi:10.7150/jca.31464[Crossref]
- Devassy R, Gopalakrishnan S, De Wilde RL. Surgical Efficacy Among Laparoscopic Ultrasonic Dissectors: Are We Advancing Safely? A Review of Literature. J ObstetGynaecol India. 2015;65(5):293–300. doi:10.1007/s13224-015-0774-x[Crossref]
- In SM, Park DY, Sohn IK, Kim CH, Lim HL, Hong SA, Jung DY, Jeong SY, Han JH, Kim HJ.Experimental study of the potential hazards of surgical smoke from powered instruments.Br J Surg. 2015 Nov; 102(12):1581-6.[Crossref]
- Kim FJ, Sehrt D, Pompeo A, Molina WR. Comparison of surgical plume among laparoscopic ultrasonic dissectors using a real-time digital quantitative technology. SurgEndosc. 2012;26(12):3408–3412. doi:10.1007/s00464-012-2351-z[Crossref]
- Resources for Smoke & Gas Evacuation During Open, Laparoscopic, And Endoscopic Procedures. March 31, 2020 by EAES- SAGES joint recommendations. Available at https://eaes.eu/resources-on-smoke-gas-evacuation-during-open-laparoscopic-and-endoscopic-procedures/
- Mintz Y, Arezzo A, Boni L, Chand M, Brodie R, Fingerhut A and the Technology Committee of the European Association for Endoscopic Surgery. A Low Cost, Safe and Effective Method for Smoke Evacuation in Laparoscopic Surgery for Suspected Coronavirus Patients. Annals of surgery 2020 April.[Crossref]
- Personal Protective Equipment (PPE) to protect you from COVID-19. What to wear and when. Available at https://icmanaesthesiacovid-19.org/.
- Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection [published online ahead of print, 2020 Apr 5]. EClinicalMedicine. 2020;100331. doi:10.1016/j.eclinm.2020.100331[Crossref]
- Tobón GJ. Ospina FE, PabloSuso J, et.al. Autoantibodies production and immunological abnormalities after bariatric surgery. Journal of Translational Autoimmunity 2019 Dec. https://doi.org/10.1016/j.jtauto.2019.100024