Abstract
Background: The first reported death among homeless persons in Miami Dade County was a 26-year-old male who presented with a fever at one of the free clinics in Homestead, Florida, and was immediately transported to the nearest public hospital in the area where he later died from COVID-19. Since that first death, other homeless persons have died from COVID-19. The purpose of this paper is to report the impact of congregant living in two homeless shelters and a free clinic’s response to COVID-19 in south Florida.
Problem: Homeless and underserved populations in South Florida are faced with medically complex needs that are partially met by onsite clinics. Unfortunately, the COVID-19 pandemic has further limited access to onsite clinic and hospital outpatient services. Therefore, follow up care and recovery support are minimal and adversely impact quality of life, resulting in a cost burden to the healthcare system.
Methods: Nasopharyngeal swabs were collected daily, Monday through Friday, from homeless persons living in and around the two shelters for 3-months, along with persons identified through contact tracing. All samples were tested for COVID-19 by reverse transcription polymerase chain reaction with results reported from the local Department of Health (DOH) laboratory.
Interventions: To decrease the spread of COVID-19, any shelter homeless person reporting symptoms or suspected of being positive for COVID-19 was assessed, tested, and separated from other residents until confirmation results were delivered. If positive, the resident was quarantined for 14-days in a single-room hotel designated for homeless persons testing positive for SARS-CoV-2, the virus that causes COVID-19.
Results: The clinic staff, assisted by the local DOH, conducted 545 coronavirus tests to 408 sheltered and unsheltered homeless persons living in and around the two shelters. Of the 545 tests performed, 56 (10%) were positive, 458 (84%) were negative, 44persons recovered from COVID-19, 4 (1%) persons died, 2 (<1%) persons were re-infected with COVID-19, 23 patients were hospitalized during the period of this study, and 108 persons were placed in quarantine, which included persons exposed during contact tracing.
Conclusion: Due to a lack of follow up, many homeless persons become super spreaders of COVID-19. Unless timely interventions using face coverings, quarantine, social distancing, and frequent hand washings are initiated, the spread of COVID-19 will continue among homeless persons resulting in greater morbidity and mortality among this population.
Keywords
Homeless, COVID-19 outbreak, Homeless shelters, Homeless clinics
Introduction
COVID-19 has taken the lives of over 1,305,189 people world-wide and greater than 244,250 in the U.S. In addition, confirmed global COVID-19 cases have reached 53,517,017 in 191 countries/regions, and in America, over 10.8 million confirmed cases [1]. As of November 14, 2020, Florida has the 3rd highest number of positive cases behind Texas and California, and reported 877,933 positive COVID-19 cases and 17,517 deaths [2]. Miami-Dade (MDC) and Broward (BC) counties lead the state in the number of positive cases and deaths, with MDC reporting 200,876 cases and 3,711 deaths, and BC reporting 95,371 cases and 1,592 deaths [1,2]. Included in the reported cases and death tolls are homeless persons adversely affected by COVID-19. The Miami Rescue Mission (MRM) provide shelter services to over 2000 homeless persons annually.
Background
The first reported death among homeless persons in MDC was a 26-year-old male who presented with a fever at one of the free clinics in Homestead, Florida, and was immediately transported to the nearest public hospital in the area where he later died from COVID-19 [3]. Homeless individuals and families are at increased risk for contracting and transmitting COVID-19, as well as other communicable diseases. Due to poor living conditions and limited access to healthcare resources, homeless people of all ages are vulnerable to acquiring COVID-19. This article will address measures taken to protect homeless men and women residing in local homeless shelters from the spread and increased morbidity and mortality associated with COVID-19 in south Florida.
History
The Miami Rescue Mission Clinic (MRMC) is a free clinic that provides primary medical services to over 11,000 homeless, destitute, uninsured, underinsured and underserved populations in south Florida annually. The MRMC has had a consistent presence in the South Florida community since 2009, addressing basic healthcare needs of homeless persons by assisting them in navigating through complex healthcare systems when additional care is needed, obtaining the necessary resources with area specialists and local hospitals, and facilitating lasting medical improvement toward empowering the patients to manage and take control of their own healthcare needs. All services including labs, medications, referred specialists and more sophisticated care arranged are provided at no cost. The MRMC is associated with the MRM, a homeless shelter, that is geographically located across the street from each other in one of the most underserved areas in South Florida, where one would find at any time of the day, homeless men and women sleeping on the sidewalks adjacent to both the MRM and the MRMC. A similar picture is seen in South Broward County (BC) at our MRM Broward Outreach Center (BOC). The MRM, Inc. is a not-for profit, 501c3 corporation that has provided meals, shelter, life-changing programs, and hope to men, women and children in need since 1922. The MRM onsite services include low demand shelter beds (24-hour – 7-days-a-week residential stay), overnight beds, three daily meals, transitional housing, case management, workforce development, life skills, health care, and stabilization services. In 2019, the MRM provided over 900,000 meals, an increase of 300,000 meals from 2018 and over 600,000 nights of safe shelter to people in need, living in MDC and BC.
COVID-19
COVID-19 is a human coronavirus frequently associated with upper respiratory tract infections (URTIs), but can also cause lower respiratory tract infections (LRTIs), such as pneumonia or bronchitis due to inflammation of the lung parenchyma [4,5]. The coronaviruses are positive-stranded ribonucleic acid (RNA) viruses named for their appearance as seen under an electron microscope, which shows elliptic virion projections of corona (crown-like spikes) from the Latin word for crown [4,6-8]. Prior to 2002, coronaviruses contributed 10% to 30% of the common colds and did not cause severe harm to humans [9,10]. However, since the outbreak of SARS-CoV in 2002 and MERS-CoV in 2012, genetic mutations of these coronaviruses resulted in severe respiratory illnesses when attached to human proteins in human respiratory tracts as well as increased mortality rates stemming from associated pulmonary and coronary emboli [9,11,12]. The World Health Organization (WHO a) issued the interim name “2019-n-CoV” on February 11, 2020, because it originated in the year 2019, the “n” indicating novel, and the “CoV” referring to coronavirus, categorizing the virus under SARS-CoV-2, later to COVID-19 [6,13]. COVID-19 is known to spread from person-to-person, between people who are in close contact with one another (less than 6 feet apart), through respiratory droplets, and touching contaminated items or inanimate surfaces [14]. It is also known that measures to prevent the spread of COVID-19, require proper hand-washing, use of personal protective equipment, social distancing of 6-feet apart, covering mouth and nose when coughing or sneezing, proper disposal of tissues, and properly cleaning frequently used surfaces with Food and Drug Administration (FDA) approved cleaning and disinfecting solutions [14,15]. Initially, due to limited personal protective equipment (PPEs) and close living conditions, the MRMC and the MRM shelters worked closely together to quickly address the Centers for Disease and Prevention (CDC) recommendations on preventing the spread of COVID-19 in our facilities [14].
The Problem
To protect MRM shelter residents from the spread of COVID-19 during the incubation period when residents were free of viral infection symptoms and viral antigen testing had not begun, MRMC staff initiated educational seminars emphasizing social distancing, frequent hand washing and importance of identifying and reporting symptoms of fever, cough, and difficulty breathing immediately to their case worker and clinic staff. The MRM also implemented strategic interventions by not allowing any new homeless admissions to either site location, spacing the beds in each dorm to at least six feet apart, providing hand sanitizers and disposable wipes to all residents, and cleaning frequently touched surfaces with FDA approved disinfectants [15]. The local health department was contacted to assist in providing antigen testing for all MRM shelter residents. Also, during the early outbreak of COVID-19 in South Florida, clinic and shelter staff closely monitored levels of transmission in MDC and BC knowing that the homeless population served has a higher risk of increased exposure and continuing disease transmission because of the large numbers of people living together.
MRM Clinic Rapid Response to COVID-19
To maintain disease surveillance and control, the MRMC and MRM staff worked twenty-four hours on-call to respond to any reported COVID-19 symptoms, with the understanding that presenting symptoms of fever, cough, shortness of breath or general malaise may be the only indication of the onset of COVID-19 [8,16]. It was equally important to initiate quarantine efforts if indicated, as we differentiated COVID-19 signs and symptoms from that of the flu virus and allergy symptoms. Understanding the incubation period for a virus helped to determine the quarantine period necessary to prevent and control viral spread [12,16]. According to the WHO, the incubation period for COVID-19 is between 2 to 10 days [7]. The main symptoms of COVID-19 are fever, tiredness, cough, and shortness of breath [8,15,16]. However, allergy symptoms are more chronic and present with sneezing, itching (eyes or skin), wheezing, post nasal drip, and coughing [16-18]. The flu virus may present with symptoms similar to COVID-19, but usually do not involve shortness of breath, except if the lower respiratory system has become involved and the condition has worsened. Common signs and symptoms of the flu virus include fever and chills, runny nose or nasal congestion, cough, occasional sore throat, myalgia, fatigue, headaches and body aches [19]. Residents reported to MRMC showing any of the symptoms listed were tested for COVID-19, and if positive, immediately quarantined in a local hotel, single person occupancy, for fourteen (14) days. At the end of the quarantine period, residents were retested for the antigen and if negative, returned to their dormitory at the MRM shelter. If a resident retested positive, the 14-day quarantine was repeated. Those residents who tested negative, but presented with symptoms were advised to stay in their dorm rooms until symptoms subsided and appropriate treatment plans were initiated. For those with more serious symptoms such as breathing difficulties, elevated temperature, and a productive cough (which can indicate pneumonia and warrant immediate medical attention) were seen by the health care provider (physician, physician assistant, or advanced practice registered nurse) via telehealth and transported by local fire and rescue services or the MRM transport van (depending upon the critical physical state of the patient) to the nearest local emergency care center for further evaluation and management. In an ongoing effort to maintain the health and well-being of the MRMC patients, the MRMC dispensed over 500 medications to homeless patients living at one of the MRM-BOC shelters over a two-month period.
Methods
First, adjustments made by the MRMC to the COVID-19 pandemic involved a rapid transition to telehealth for residential clients. Second, clinic staff provided urgent primary care to clients after local hospitals, clinics and community health centers cancelled the majority of specialty care visits, such as mental health and other critical services. Third, clinic staff provided patient medication refills delivered to the shelters to decrease emergency room utilization and a greater financial impact of existing stressed health care services due to COVID-19. Fourth, COVID testing and re-testing was initiated by the MRMC staff assisted by the local Department of Health (DOH). COVID-19 testing was conducted using nasopharyngeal swabs daily, Monday through Friday, from homeless persons living in and around the two shelters for 3-months, along with persons identified through contact tracing. COVID test results of homeless persons tested was provided by the DOH laboratory. Nasopharyngeal swabs were used because the research has shown that larger amounts of positive COVID-19 virus and viral RNA can be detected early in the disease using nasopharyngeal samples rather than throat swabs, and is independent of symptom presentation or severity [20,21]. Fifth, after clinic hours ended, clinic and shelter providers coordinated their efforts to verify priority patient needs, creating social distancing in dormitories and a single-use area in the clinic, reviewing client documentation (identifications, medical records, and symptoms) to determine the need for quarantine. Sixth, care coordination for contact tracing with local health department officials was ongoing. Seventh and ongoing was the reentry of quarantined patients back to the facility, avoiding stigmatization of previously affected individuals, and addressing the COVID deaths of clients. These action steps were taken in a rapid-fire format to reduce the spread of COVID-19 among the homeless population served. Studies have shown that viral shedding in respiratory secretions are common and can occur up to 3-days before the first clinical symptoms appear [22,23].
Interventions
The MRMC closed its clinic doors at the peak of the COVID-19 pandemic in response to mandatory shutdown orders by Florida’s Governor Rick DeSantis of non-essential businesses and orders for social distancing and face covering requirements of essential businesses for about 2-days to allow for increased purchasing of personal protective equipment (PPEs) for staff and patients and to create a social distancing design in the clinic. Following several coordinated MRMC health care and primary care providers (HCPs/PCPs) and MRM staff meetings and telehealth trainings, telehealth visits were initiated by having the on-call or on-site provider to log-in to the MRMC electronic medical record system (EMRS) and a web-video conferencing platform that is accessed by patients at each of the shelters in a designated area for private consultation. The web-video conferencing telehealth sessions allow the HCPs or PCPs and patients to connect using technology to deliver required health care services.
Telehealth
The Telehealth format allowed for synchronous (real-time telephone or live audio-video interactions with the patient using a smartphone, tablet, or computer). The caseworker/on-site medical technician was equipped with marginal medical equipment, such as temporal thermometers, digital blood pressure machines, weight scales, and oxygen saturation finger monitors. Biometric and anthropometric readings were obtained and reported by the onsite shelter medical technician while the consulting PCP conducted the remote evaluation and documented findings and planned treatments in the EMR. The MRMC PCPs conducted 397 telehealth visits over a 3-month period (June to September, 2020). Although, asynchronous (technology where messages, images, or data are collected at one point in time and interpreted or responded to later) and remote patient monitoring (direct transmission of a patient’s clinical measurements from a distance in real time or post-dated times to the PCP) are available, these two modalities were not used [24]. However, MRMC staff provided daily telephone welfare checks (362) over the same 3-month period to patients placed in quarantine at hotels or to those persons with symptoms of upper respiratory tract conditions, but tested negative or was diagnosed with other co-morbid conditions that warranted close follow-up. Because all clinic services are free, MRMC did not receive any telehealth reimbursement using the International Classification of Diseases (ICD) code – 10 99211 for office or other outpatient visits or Current Procedural Terminology (CPT) code – 99371 for telephone call by a physician to patient or for consultation or medical management or for coordinating medical management with other [25,26]. By quickly implementing Telehealth in the MRMC and making it available to homeless shelter residents, transmission of COVID-19 and other preventable diseases were mitigated, providing a safer option for HCPs, PCPs, and the patients served.
Results
The MRMC HCPs assisted by the local DOH staff, provided 545 coronavirus testing to 408 sheltered and unsheltered homeless persons living in and around the MRM and BOC persons and conducted 362 wellness telephone encounters (Table 1). Of the 545 tests performed, 56 (10%) were positive, 458 (84%) were negative, 44 persons recovered from COVID-19 (which includes individuals that tested negative and were added to the contact tracing), 4 (1%) persons died, 2 (<1%) persons were re-infected with COVID-19, 23 patients were hospitalized during the period of this study, and 108 persons were placed in quarantine, which included persons exposed during contact tracing. Ninety patients were tested at least two times during this study and one patient tested positive three times (15 Days after the first positive test and 7 days after the second positive test), The negative test for this patient came after 42 days after the first positive test.
Table 1: COVID-19 Testing Information.
|
Tests |
N |
% |
|
N. of Tests performed Outcome |
545 |
100.0% |
|
Positive |
56 |
10.3% |
|
Negative |
458 |
84.0% |
|
Lab/STD |
31 |
5.7% |
Most of the individuals tested were male (83.6%, 341 Individuals), see Figure 1 and the average age of the individuals tested were 47.7 years. Regarding race and ethnicity, 74% of the patients were black and non-Hispanic (327 patients, 80%) (Table 2, Figures 2 and 3), 96% of the patients who tested positive were male and their average age was 49.3 years; 60% were black and 64% reported no Hispanic origin (Table 3), 23 patients were hospitalized and 4 died due to COVID-19. All 27 patients were male with an average age of 55.1 years (Table 4). The average age of patients who were hospitalized were 53.1 years, while the average age of the deceased patients and were on average 55.2 years old. The ages of the 4 victims who passed away ranged between 56 to 74 years of age.
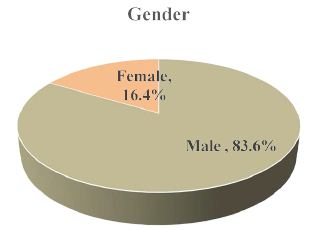
Figure 1: Demographics of Homeless Persons Tested for COVID-19 by Gender.
Table 2: Patient Demographics who were Tested for COVID-19.
|
Demographic Characteristics |
N | % |
| Number of Patients | 408 |
100.0% |
|
Age |
||
| Mean Age ± SD |
47.7 ±14.6 |
|
|
Gender |
||
| Male | 341 |
83.6% |
|
Female |
67 | 16.4% |
| Race and Ethnicity | ||
|
Black |
303 | 74.3% |
| Hispanic |
3 |
|
|
Non-Hispanic |
300 | |
| White | 104 |
25.5% |
|
Hispanic |
78 | |
| Non-Hispanic |
26 |
|
|
Asian |
1 | 0.2% |
| Hispanic Origin | ||
|
Hispanic |
81 | 19.9% |
| Non-Hispanic | 327 |
80.1% |
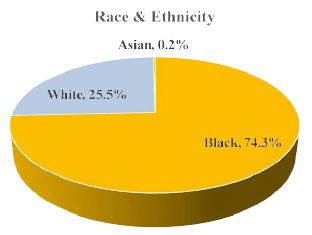
Figure 2: Demographics of Homeless Persons Tested for COVID-19 by Race.
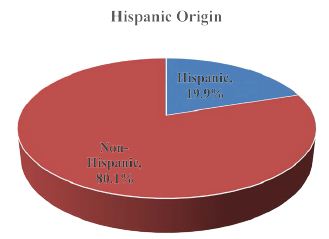
Figure 3: Demographics of Homeless Persons Tested for COVID-19 by Ethnicity.
Table 3: Patient Demographics who Tested Positive for COVID-19 at least in one test.
|
Demographic Characteristics |
N | % |
| Number of Patients | 53 |
100% |
|
Age |
||
| Mean Age ± SD |
49.34 ± 12.9 |
|
|
Gender |
||
| Male | 51 |
96.2% |
|
Female |
2 | 3.8% |
| Race and Ethnicity | ||
|
Black |
32 | 60.4% |
| Hispanic |
0 |
|
|
Non-Hispanic |
32 | |
| White | 21 |
39.6% |
|
Hispanic |
19 | |
| Non-Hispanic |
2 |
|
|
Hispanic Origin |
||
| Hispanic | 19 |
35.8% |
|
Non-Hispanic |
34 |
64.2% |
Table 4: Patient Demographics and Presenting Symptoms who were Hospitalized or Died due to COVID-19.
|
Demographic Characteristics |
N | % |
| Number of Patients |
27 |
|
|
Age |
||
| Mean Age ± SD |
55.15 + 10.6 |
|
|
Gender |
||
| Male | 27 |
100.0% |
|
Female |
— | |
| Race and Ethnicity | ||
|
Black |
23 | 85.2% |
| Hispanic |
— |
Among the four deaths from the homeless shelter, three were confirmed COVID-19 positive and one unconfirmed. The three confirmed COVID-19 deaths occurred within 6-days of each other. Each victim had preexisting conditions and were being treated at the MRMC prior to hospitalization for a history of diabetes mellitus, obesity and hypertension. The fourth homeless death occurred one-month following the first three deaths and was unconfirmed for COVID-19. All victims were males, three were non-Hispanic Blacks and one Hispanic. Each of the three deaths presented to the emergency room with shortness of breath, fever and cough; admitted to the intensive care unit where their conditions deteriorated rapidly; and decompensated requiring increased oxygen and later intubation.
Contact Tracing, Quarantine and Reentry
Contact tracing plays a significant role in identifying positive cases, interrupting viral transmission and helps to prevent further spread of the virus. Contact tracing involves four-steps: (1) case investigation of close contacts, (2) contact tracing of exposed individuals, (3) contact support through education, information and exposure reduction, and (4) self-quarantining by staying at home and maintaining social distancing of at least 6-feet for th14-days [27]. MRMC HCPs conducted contact tracing on 108 patients. Of the 108 patients, 65 tested positive for COVID-19 and were placed in quarantine at the designated hotel. All hotel rooms used for housing positive COVID-19 patients were properly decontaminated using FDA approved disinfecting agents. Patients quarantined were required to wear face coverings when exiting the room for individual meals, when in contact with family members during the quarantine period, and when outside or in close contact with other people. Asking everyone to wear masks has helped to reduce the spread of COVID-19 by persons who may be unaware that they have the virus [16,27]. The N95 and KN95 masks are both rated to capture 95% of particles. The KN95 masks are made in China and require wearers to pass a fit test [28]. The N95 masks produced by the 3M company have stronger breathability standards. However, both the KN95 and the N95 mass filtration efficiency captures salt particles and a tested flow rate of 85L/minute [28]. Surgical masks provide approximately 63% filtration and cotton hander kerchiefs provide about 28% filtration [28]. It has been reported that “several 3M masks were able to capture over 99% of tiny 0.01-micron particles (10 times small than the coronavirus), even while on people’s face” [28].
Management and Treatment Options
Patients, staff, volunteers and visitors to the MRM or BOC experiencing any coronavirus disease were required to practice general prevention measures to include adequate rest and sleep, eating a well-balanced diet, washing hands frequently with a hand sanitizer (60% alcohol minimum) or soap and water for 20-seconds or longer, drying hands thoroughly with a clean towel or air dry, avoiding touching eyes, nose, or mouth with unwashed hands or after touching surfaces, covering mouth with a tissue or sleeve when sneezing or coughing, using a protective face covering, and calling the PCP before visiting the clinic. The HCPs were required to notify health authorities to assist with contact tracing as needed [27]. The foregoing requirements are essential for vulnerable populations and people of color who are disproportionately affected by COVID-19 because the virus is increasing at alarming rates among this group due to underlying health and economic disparities [29]. Data from the COVID-19 tracking project traces racial and ethnic data from reporting states across America and show that people of color account for 24% of COVID-19 deaths but represents only 13% of the U.S. population [30,31]. In a recent article by Washington & Cirilo [32] on vaccinating homeless persons, 76% of the participating population were members of an ethnic minority group and consisted of 117 non-Hispanic Blacks, 50 non-Hispanic Whites, 35 Hispanics, and 7 Haitians; with males (177) outnumbering females (32) in the active group. Currently the racial/ethnic make-up of MRMC patients are seen in Table 4.
To address early identification of COVID-19 in homeless shelter residents, the MRMC has partnered with a COVID-19 research and development company that is piloting a non-invasive pre-screening device, COVID PlusTM Monitor, that provides real-time subclinical markers for COVID-19 and can be worn by both children and adults [33]. The instrument is able to detect sub-clinical abnormalities associated with inflammatory markers that have shown strong correlation between COVID-19 and hyper-inflammatory states like hypercoagulation [33-35]. The COVID PlusTM is able to “allow healthcare providers to identify potentially infected patients, directing them to seek further testing and medical intervention, and avoiding the spread of infections among the general public” especially among homeless persons [33]. The device provides data within 3 to 5 minutes on abnormalities found in blood flow and other COVID-19 related complications and can track disease severity, progression, and recovery [33]. The COVID PlusTM device has been tested on over 1,000 COVID PCR positive subjects, using hundreds of biometric markers that identify patterns commonly associated with COVID-19 [33]. The goal established by the MRMC is early identification of COVID-19 among sheltered homeless persons. Once identified, actions can be taken to quickly quarantine those individuals to reduce the spread of COVID-19 among persons in congregant living facilities, such as a homeless shelter. The early identification also includes the essential workers who provide for their food, safety and shelter.
Vaccine Therapy
Nonetheless, homeless populations and racial/ethnic vulnerable groups are at-risk for contracting COVID-19 and would greatly benefit from increased accuracy in SARS-CoV-2 testing and a safe vaccine therapy. Now that Pfizer’s vaccine BNT162b2 has received emergency use authorization (EUA) from the FDA [36,37], it is critical that frontline healthcare workers, volunteering or employed by the Free Clinics, receive the COVID-19 vaccine in the first distribution. The CDC and U.S. Surgeon General encourage the continued wearing of face coverings, physical distancing, proper isolation, quarantine of infected individuals, and contact tracing to help us mitigate SARS-CoV-2 spread. Nonetheless, a safe and effective preventive vaccine is needed for healthcare workers and the general public to help create herd immunity against COVID-19 and to ultimately control this pandemic.
The MRMC currently has a vaccination program for the homeless and have vaccinated hundreds of homeless men and women with both pneumonia vaccines, PPSV23 and PCV13, quadrivalent Influenza, tetanus, diphtheria and acellular pertussis (Tdap), and Hepatitis C vaccines over the past five-years, reducing the incidence of vaccine preventable illnesses among the homeless population in MDC and BC [32]. A proven safe and effective COVID-19 vaccine could greatly reduce morbidity and mortality rates among disparate homeless populations. Homeless persons living in and around homeless shelters are among the most vulnerable, are considered high risk due to their multiple co-morbid conditions and transient characteristics, and should also be considered in the first or second round of vaccine therapy once made available to the general public.
Conclusion
Coronaviruses are respiratory diseases that infects older children and adults, including homeless men and women, more commonly than younger children [27,36]. The chances of dying from the virus is age dependent and influenced by the social determinants of health (where we live, eat and work), persons living in crowded facilities such as homeless shelters, and persons with higher comorbid conditions having worse prognoses [4,29-30]. Homeless persons and people living in poor communities with decreased access to health care and healthy foods, employment struggles, high toxic stress (allostatic loads), and factors surrounding coronaviruses, increase the risk of getting the disease and dying from the disease [29]. There were many challenges faced by homeless populations, shelters, and free clinics when the pandemic hit South Florida. The seven-step method implemented by the MRM and MRMC at the onset of Florida’s State-wide shut down may have saved more lives than the four persons that died from SARS-CoV-2. However, interventions like contact tracing and disease management were constrained due to the transient nature of the homeless population. The socio-demographics were constantly changing as individuals left the shelter and were not allowed to return during the shut-down, especially when we had minimal PPEs and test kits to protect the frontline workers and to determine positivity rates. Currently, we have an EUA approval for Pfizer’s BNT162b2 vaccine. Although frontline workers mainline employed by hospitals and long-term care facilities are receiving the vaccine first, healthcare workers assigned to provide healthcare services to the homeless must be considered as frontline workers and receive the COVID-19 vaccine. The challenges still remain to reduce hesitancy to receiving the vaccine for both healthcare workers, the general public, and homeless persons living in and around homeless shelters. More information is still needed on the safety and efficacy of the vaccine, especially when used in vulnerable populations who present with multiple co-morbid health conditions. In conclusion, homeless persons rely on health care services provided by free clinics, hospitals, and emergency rooms when they become ill. Due to the COVID-19 pandemic, the obstacles to receiving health care increased and many homeless persons with mild or undetectable symptoms are not seen by health care providers or discharged from health care facilities with minimal or no treatment. Due to a lack of follow up, many homeless persons become super spreaders of COVID-19. Unless timely interventions using face coverings, quarantine, social distancing, and frequent hand washings are initiated, the spread of COVID-19 will continue among homeless persons resulting in greater morbidity and mortality.
Acknowledgement
The authors have no conflict of interest to disclose.
References
- COVID-19 map. https://coronavirus.jhu.edu/map.html. Published November 14 2020. Accessed November 14 2020.
- Florida Department of health COVID-19 response. https://floridahealthcovid19.gov/ Published November 14 2020. Accessed November 14 2020.
- Gutierrez P, Washington-Brown L, Bretones-Graham G, Pereira-Amorim E (2020) Cardiac Related Deaths among the Homeless Persons with Covid-19: Case Presentations. International Journal of Cardiovascular Diseases and Diagnosis 5: 033-038. www.scireslit.com
- Pan A, Liu L, Wang C, Guo H, Hao, et al. (2020) Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA 323:1915-1923. [crossref]
- Woo PC, Lau SK, Chu C, Chan K, Tsoi H, Huang, et al. (2005) Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. Journal of Virology 79: 884-895. [crossref]
- World Health Organization. WHO | International Classification of Diseases, 11th Revision (ICD-11). 2020a. Retrieved from https://www.who.int/classifications/icd/en/ World Health Organization. Coronavirus disease (COVID-19) outbreak. Retrieved February 14, 2020, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- World Health Organization. 2020b, January 10. Coronavirus; Current novel coronavirus (2019-nCoV) outbreak. Retrieved February 15, 2020, from https://www.who.int/health-topics/coronavirus
- Vassilara F, Spyridaki A, Pothitos G, Deliveliotou A, Papadopoulos, A (2018) A Rare Case of Human Coronavirus 229E Associated with Acute Respiratory Distress Syndrome in a Healthy Adult. Case Reports in Infectious Diseases 1-4.
- Casey, G. Coronavirus – a developing outbreak (2020) Kai Tiaki Nursing New Zealand, , 26(1), pg: 26. http://db03.linccweb.org/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=141750278&site=ehost-live&scope=site
- Hand J, Rose E, Salinas A, Lu X, Sakthivel SK, et al. (2018) Severe respiratory illness outbreak associated with human Coronavirus NL63 in a long-term care facility. Emerging Infectious Diseases 24: 1964-1966. [crossref]
- Chen T, Wu D, Chen H, Yan W, Yang D, et al. (2020) Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ.
- Washington-Brown LJ, Cirilo R (2020) Coronavirus Disease – 2019-nCoV (COVID-19). Journal National Black Nurses Association 31: 19-25.
- Sauer, L. M. What is coronavirus? Health. https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus. Accessed February 11 2020.
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19): How to protect yourself and others. Retrieved February 13, 2020, from https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html.
- S. Food and Drug Administration (FDA). Important Information on the Use of Serological (Antibody) Tests for COVID-19 – Letter to Health Care Providers | FDA. (2020, June 19). Retrieved from https://www.fda.gov/medical-devices/letters-health-care-providers/important-information-use-serological-antibody-tests-covid-19-letter-health-care-providers.
- Backer JA, Klinkenberg D, Wallinga J (2020) Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travelers from Wuhan, China, 20–28 January. Eurosurveillance: European Communicable Disease Bulletin [crossref]
- Centers for Disease Control and Prevention. Symptoms of Coronavirus|CDC. 2020. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- Asthma and Allergy Foundation of America [AAFA] n.d. Allergy symptoms. https://www.aafa.org/allergy-symptoms/.
- Centers for Disease Control and Prevention. Flu symptoms & diagnosis. 2020, September 2. https://www.cdc.gov/flu/symptoms/
- Fu Y, Han P, Zhu R, Bai T, Yi J, et al. (2020). Risk factors for viral RNA shedding in COVID-19 patients. Eur Respir J [crossref].
- Tan F, Wang K, Liu J, Liu D, Luo J, et al. (2020) Viral Transmission and Clinical Features in Asymptomatic Carriers of SARS-CoV-2 in Wuhan, China. Front Med (Lausanne) [crossref]
- He X, Lau EHY, Wu P, (2020) Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med , 26: 672-675.
- Lee S, Kim T, Lee E, Lee, C, Kim H, et al. (2020) Clinical Course and Molecular Viral Shedding Among Asymptomatic and Symptomatic Patients With SARS-CoV-2 Infection in a Community Treatment Center in the Republic of Korea. JAMA Intern Med. 180:1447-1452.
- Centers for Medicare and Medicaid Services [CMS] Telehealth. 2020 April 24. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth
- American medical Association [AMA]. CPT® overview and code approval. 2019, 25. https://www.ama-assn.org/practice-management/cpt/cpt-overview-and-code-approval
- Centers for Disease Control and Prevention. ICD – ICD-10-CM – International classification of diseases, icd-10-CM/PCS transition. Centers for Disease Control and Prevention. 2019, March 1. Accessed September 2020, https://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19); Interim infection prevention and control recommendations for patients with confirmed 2019 Novel Coronavirus (2019-nCoV) or persons under investigation for 2019-nCoV in healthcare settings. 2020c, February 12. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/infection-control.html
- Alizargar J (2020) Wearing masks and the fight against the novel coronavirus (COVID-19). Pulmonology. [crossref]
- Johnson A, Buford T (2020) Early Data Shows African Americans Have Contracted, Died of Coronavirus at an Alarming Rate. www.medscape.com.
- COVID Tracking Project | The COVID Tracking Project. 2020, Retrieved from https://covidtracking.com/
- National Geographic. African Americans struggle with disproportionate COVID death toll. Retrieved from https://www.nationalgeographic.com/history/2020/04/coronavirus-disproportionately-impacts-african-americans.
- Washington-Brown LJ, Cirilo R (2020) Advancing the health of homeless populations through vaccinations. Journal of the American Association of Nurse Practitioners. [crossref]
- COVID PlusTM Monitor. 2020, https://www.tigertech.solutions/
- Chen T, Chen H, Yan W, Yang D, Chen G, et al. (2020). Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ, m1295. 2020.
- Wu C, Chen X, Cai Y, Xia J, Zhou X, (2020) Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneusmonia in Wuhan, China. 2020, JAMA Internal Medicine 180: 934-943. [crossref]
- Lai C, Shih T, Ko W, Tang H, Hsueh, P (2020) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents [crossref]
- U.S. Food & Drug Administrations (FDA). Pfizer-BioNTechCovid-19 Vaccine EUA letter of Authorization (11 December 2020). https://www.fda.gov/media/144412/download