Abstract
Background: Clear Cell Sarcoma Gastrointestinal Tumour (CCSGIT) is a rare malignant soft tissue sarcoma which is exceptionally localized in the caecum. Due to its nonspecific symptoms the diagnosis is often late and prognosis is poor. The definitive diagnosis requires a combination of morphological, immunohistochemical and molecular techniques, with positive S100 protein marker and negative for melanocytic markers. Genetic studies show EWSR1 rearrangements in all the cases. Surgical resection is the prior treatment, as neither radiotherapy nor chemotherapy appears to be effective, with average 2-year survival after thediagnosis.
Cases Summary: We present two patients, a 41 year-old male and a 36 years-old female, who presented with acute intestinal pain and obstruction, rectal bleeding and anaemia. Both of them underwent an urgent hemicolectomy. The presence of a S100 positive protein and ESWR1 rearrangements in immunochemical and molecular studies confirmed the CCSGIT diagnosis. Postoperative chemotherapy was administrated in both cases. Both patients required a second surgery: In the first patient the second surgery was required for resection of residual aortomesenteric metastatic nodes, and hepatic metastases on the second patient. Both patients died, 4 and 12 months respectively after surgical treatment.
Conclusion: CCSGIT is a distinctive soft tissue sarcoma with nonspecific gastrointestinal symptoms, late diagnosis and poor prognosis. It mainly affects young adults and the incidence of metastatic disease at the time of diagnosis is high. Its diagnosis is based on the presence of positive S100 protein and EWSR1 gene rearrangements. The Melan A, HMB-45 and C-kit are negatives. Early diagnostic and therapeutic strategies are required to provide the best clinical care leading to long-term survival. These reported cases describe two CCSGITs of primary caecum origin; which can contribute to the development of future targeted therapies as well as offering epidemiological evidence on prevalence and prognosis.
Keywords
Caecum, C-kit, Clear cell sarcoma, EESR1 genetic rearrangements, HMB-45, Malignant gastrointestinal sarcoma, Melan A, surgical treatment, S100 protein
gCore tip: Clear cell sarcoma of gastrointestinal tract is a very rare and infrequent tumour. Classically, it can be confused with other similar tumours such as melanocytic tumours, neuroectodermaltumours and gastrointestinal stromal tumours (GIST). Their immunohistochemical characteristics are based on the presence of a positive S100 protein and negative markers for HMB-45, Melan A and GIST (CD117, DOD-1 and CD34). Other important characteristics for the diagnosis of this tumour are positive EWSR1 gene rearrangements by FISH technique studies. Frequently, the CCSGITs affect children and young adults. They are highly aggressive tumours that commonly reoccur with widespread metastatic nodal and visceral disease, even after treatment. The most frequent intestinal locations are the stomach or small bowel. Colonic location and specifically the caecum is rarely described in the literature. Nowadays the only treatment is surgical resection. However, the prognostic is bad and the overall global survival at 3 years is very low. In the future, it is possible that new targeted therapies would offer a possible better prognostic for patients with this rare sarcoma disease.
Introduction
Clear Cell Sarcoma of Gastrointestinal Tumour (CCSGIT) is a rare malignant neoplasm that originates in the wall of the stomach, small intestine or large bowel. This type of tumour is more frequent in paediatric ages and young adults, and was first described in subcutaneous tissue, tendons and aponeurosis [1-4]. In 1993, Ekfors et al. reported the first case of primary gastrointestinal CCS arising in the duodenum tract4. As of today only about 40 cases have been reported and most of these originated in the stomach and small bowel. Exceptionally, only four cases have been described in primary colon origin [5-8]. In this report we present two cases of CCSGIT originated in the ascendant colon (caecum), with an exceptional clinical occlusive presentation. We carried out a literature review with special emphasis on all diagnostic and therapeutic considerations.
Case Reports
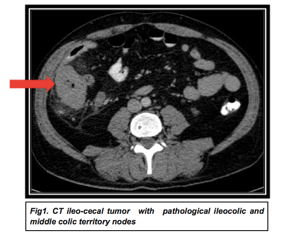
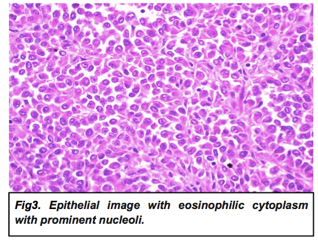
Between 2015 and 2020 two patients, a 36 year-old female and a 41 year-old male, presented clinical signs of intestinal obstruction. Both showed abdominal pain and distension, history of rectal bleeding and anaemia. In both of them the abdominal CT scan revealed the presence of a tumour located in the caecum, with infiltration of surrounding fat and thickening of the adjacent peritoneum (fig 1). The CT also detected multiple suspicious metastatic mesenteric nodes that showed pathological uptake in the PET-CT that confirmed peritumoral nodal spread (fig 2). The colonoscopy identified a neoformative process in the caecum and the biopsy was positive for malignant tumour cells with eosinophillic cytoplasm and eccentric nucleus (rabdoid phenotype). Tumour cells were positive for vimentin, keratin AE1/AE3, EMA and S100 protein and negative for keratin CAM 5.2, Melan A, HMB 45, CD45 and DOG-1. A right hemicolectomy with regional lymphadenectomy was performed and reconstruction of the intestine with an ileocolic anastomosis.
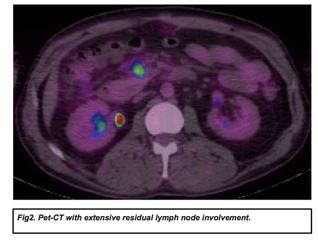
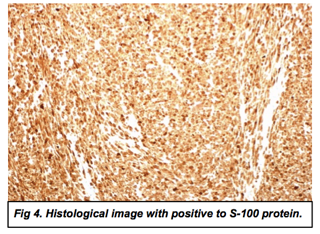
Definitive histopathological studies showed in both cases a caecum tumour with infiltration of the wall and mucosa ulceration with affection of the muscularispropia layer and the adjacent adipose tissue. The tumour showed extensive vascular and perineural invasion nests with pseudopapillary focal pattern with a predominance of epithelial cells (with fusiform areas) with eosinophilic cytoplasm that clearly rejected the periphery with prominent nucleoli compatible with a clear cell sarcoma (fig 3). Immunohistochemical studies were positive for S100 protein, CD68 and vimentin and weakly for cytokeratin CAM 5.2, LCA8CD45), DOG-1, C-kit, chromogranin, alpha-actin, desmin, HMB-45, Melan A and myeloperoxidase (fig 4). The study of gene rearrangements by FISH technique was positive for EWSR1 gene in both patients and confirming the diagnosis of Clear Cell Sarcoma (CCS) tumour. The first patient underwent adjuvant chemotherapy treatment with 5 cycles of Adriamycin 75mg/m2 with partial response and persistence of metastatic lymph nodes. Finally, resource surgery with extended mesenteric and paraaortic lymphadenectomy was performed. The new pathological study confirmed extensive residual nodal involvement with the same initial diagnosis of CCS. In the second male patient liver metastases were detected in sequential postoperative CTs and a posterior partial hepatic surgical resection was done. Both patients developed important extensive ganglion and diffuse metastatic disease and died eight and twelve months after surgery.
Discussion
Clear Cell Sarcoma of Gastrointestinal Tract (CCSGIT) is a very infrequent tumour and until 2015 only 40 reports had been published. However only 16 of this reports described tumours that corresponded with the accepted morphological, structural and immunochemical features of a CCSGIT. The most common localization is the small bowel; the stomach and the colon are more rarely affected [1-6]. CCS is more frequent in paediatric and young to middle age adults with reported median age of 40 years (from 17 to 77) [5,6]. There seems to be an equal distribution between the sexes. The most common signs and symptoms are similar to those attributed to gastrointestinal tumours: abdominal pain, intestinal distension or obstruction, gastrointestinal bleeding and anaemia. The unspecific clinical presentation and consequent delayed diagnosis play a key role in the definitive prognosis [5-10].
This rare tumour is a source of diagnostic dilemma as it shows features of melanocytic differentiation. The main diagnosis technique for accurate diagnosis is based on its histology and immunohistochemistry, but these approaches do not distinguish between malignant melanoma and CCSGIT. CCSGIT has a histological appearance that is strikingly similar to metastatic melanoma, and also needs to be differentiated from Gastrointestinal Stromal Tumours (GIST) and poorly differentiated papillary adenocarcinoma. The tumour cells of CCSGIT are predominantly epitheloid with oval or round nuclei and a variable amount of eosinophillic or clear cytoplasm, as observed in our patients, but a case featuring oncocytic cytoplasm has been reported [10]. The nuclei display an irregular nuclear contour. Nucleoli are inconspicuous but occasionally prominent and basophilic. Necrosis and surface ulceration can be seen. Osteoclast-like multinucleated giant cells are a frequent and consistent finding. Metastatic tumours resemble the primary tumour morphological features, including the presence of osteoclast-like multinucleated giant cells. All the metastatic nodes in our patient with the extended lymphadenectomy showed the same histopathology as the primary tumour.
From an immunohistochemical point of view, it is well accepted that CCSGITs are characterized by strong and diffuse staining for the S100 protein. In addition these tumours tend to lack melanocytic specific markers including HMB-45, Melan A, Thyrosinase and macrophtalmic associate transciptor factor (MITF) [8] and they do not express GIST markers (CD117,DOG1 and CD34) [4]. Another important finding is that the EWSR1 gene rearrangements are present in CCSGITs. Antonescu et al team studied three cases of CCSGI and claimed to be the first to describe a recurrent translocation of EWS (22q12) and CREB1(2q32.3) resulting in EWS-CREB1 fusion: they concluded that these cases may present a gastrointestinal neuroectodermaltumour that expresses neuroectodermal markers and a lack of melanocytic differentiation. However, the existence of rare cases of CCSGIT with EWS-ATF-1 gene fusion that also lack melanocytic differentiation supports the theory of a common histogenesis between the two tumours [6, 11]. In our two patients the tumours were positive for S100 protein and expressed some neuroectodermal markers but lacked melanocytic differentiation. The study of gene rearrangements by FISCH technique was positive for EWSR1 gene in both patients.
In terms of treatment, surgical excision is the main therapeutic and curative approach. However, in the majority of the series, more than 30% patients presented metastatic disease at diagnosis. The adjuvant chemotherapy and/or radiotherapy do not contribute therapeutic benefits. The majority of the patients died before 2 years after diagnosis.
Conclusion
In summary, CCSGIT is a rare tissue tumour, which usually affects tendons and aponeurosis of soft tissues. Very few cases reported this tumour in the gastrointestinal tract (CCSGIT). Among them the caecum is an exceptional localisation. CCSGI is considered an aggressive malignant neoplasm with unfavourable prognosis and most patients die within two years from the diagnosis. Clinical manifestations are very unspecific, such as abdominal pain, acute intestinal obstruction, digestive haemorrhage and anaemia, which delay diagnosis and treatment. The definitive diagnosis is based on immunohistochemicqal and genetic techniques. These studies present a positive S1200 protein with negative melanocytic or GIST markers. The EWSR1 rearrangement gene is observed in all cases. In addition, this is an aggressive sarcoma tumour and has poor prognosis. Surgical resection is the only possible curative treatment, specially if indicated early. In all of these cases the discussion of therapeutic strategies in a multidisciplinary sarcoma committee is necessary.
Acknowledgements
We would like to thank the patients for allowing their cases to be reported.
Competing Interests
The authors certify that there is no conflict of interest with any financial organisation regarding the material discussed in this paper.
References
- Zambrano E, Reyes-Mugica M, Franchi A, Rosai J (2003) An osteoclast-rich tumour on the gastrointestinal tract with features resembling clear cell sarcoma of solft parts: repotrs of 6 cases of a GIST Simulator. Int J SurgPathol11:75-81. [Crossref]
- Thway K, Judson I, Fisher C (2014) Clear cell sacoma-like tumor of the gastrointestinal tract, presenting as a second malignancy lear cell sacoma-like tumor of the gastrointestinal tract, presenting as a second malignancy afthe childhood hepatoblastoma. Case Rep Med984369.[Crossref]
- Liu C, Ren Y, Li X, Cao Y, Chen Y, et al (2014) Absence of 19 known hotspot oncogènic mutation in solft tissue clear cell sarcoma: Two cases report with review of the literatura. Int J ClinExpPathol7:5242-5249.
- Antonescu CR, Nafa K, Segal NH, Dal Clin P, Ladanyi M (2006) EWS-CREB1: A recurrent variant fusion in clear cell sacoma. Association with gastrointestinal location and abscense of melanocytic differentation.Clin Cancer Res12:5356-5362. [Crossref]
- Ekfors TO, Ku Yan H, Isomaki M (1993) Clear cell sacoma tendons and aponeurosis (malignan melanoma of solft parts) in the duodenum: the first visceral case. Histopathology 22: 255-259. [Crossref]
- Stockman DL, Miettienen M, Sister S, Spagnolo D (2012) Malignant gastrointestinal neuroectodermaltumour: clinicopathologic, inmunohistochemical , ultraestructural and molecular anàlisis of 16 cases with reappraisal of clear sarcoma-like tumors of gastrointestinal tract. AM J SurgPathol36:857-868. [Crossref]
- D’Amico FE, Ruffolo C, Romeo S, Massani M, Dei Tos AP, et al. (2012) Clear cell sarcoma of the ileum: report of a case and review of the literatre. Int J SurgPathol20: 401-406. [Crossref]
- GahanbaniA,BoyleDJ,EltonE (2016) Gastrointestinalclearcellsarcoma-likeoftheascendint colon. Ann R CollSurgEngl98: e37-e39. [Crossref]
- MoslimMA,FalkGA,CruiseM,Morris-StiffG (2016) Simultaneousclearcellsarcomasofthe duodenum and yeyunum. Case Rep Med2016: 1534029. [Crossref]
- Kong J, Li N, Wu S Guo X, Gu C, Fenf Z (2014) Malignant gastrointestinal neuroectodermaltumour: A case and review literature. OncolLett(internet) 2687-2690.
- Wang J, Thway K (2015) Clear cell sarcoma-like tumour of gastrointestinal tract: an evolving entity. Arch Pathol Lab Med 139(3):407-12. [Crossref]